Five things we still don't know about the vaccine rollout
- Published

The government says that 15m people have been vaccinated across the UK.
This means just over one in four adults have had their first dose of vaccine but there are some unanswered questions about the rollout.
1. What is the uptake in minority communities?
It appears that uptake in ethnic minority groups is lower than it is for the population as a whole.
This is despite some minority groups, including Bangladeshi and Pakistanis, facing higher coronavirus death rates than white people, external.
A survey, carried out by the University of Oxford and the London School for Hygiene and Tropical Medicine, suggested that black people over 80 were almost half, external as likely to have had the vaccine than white people over 80.
The gaps are smaller for people in their seventies.
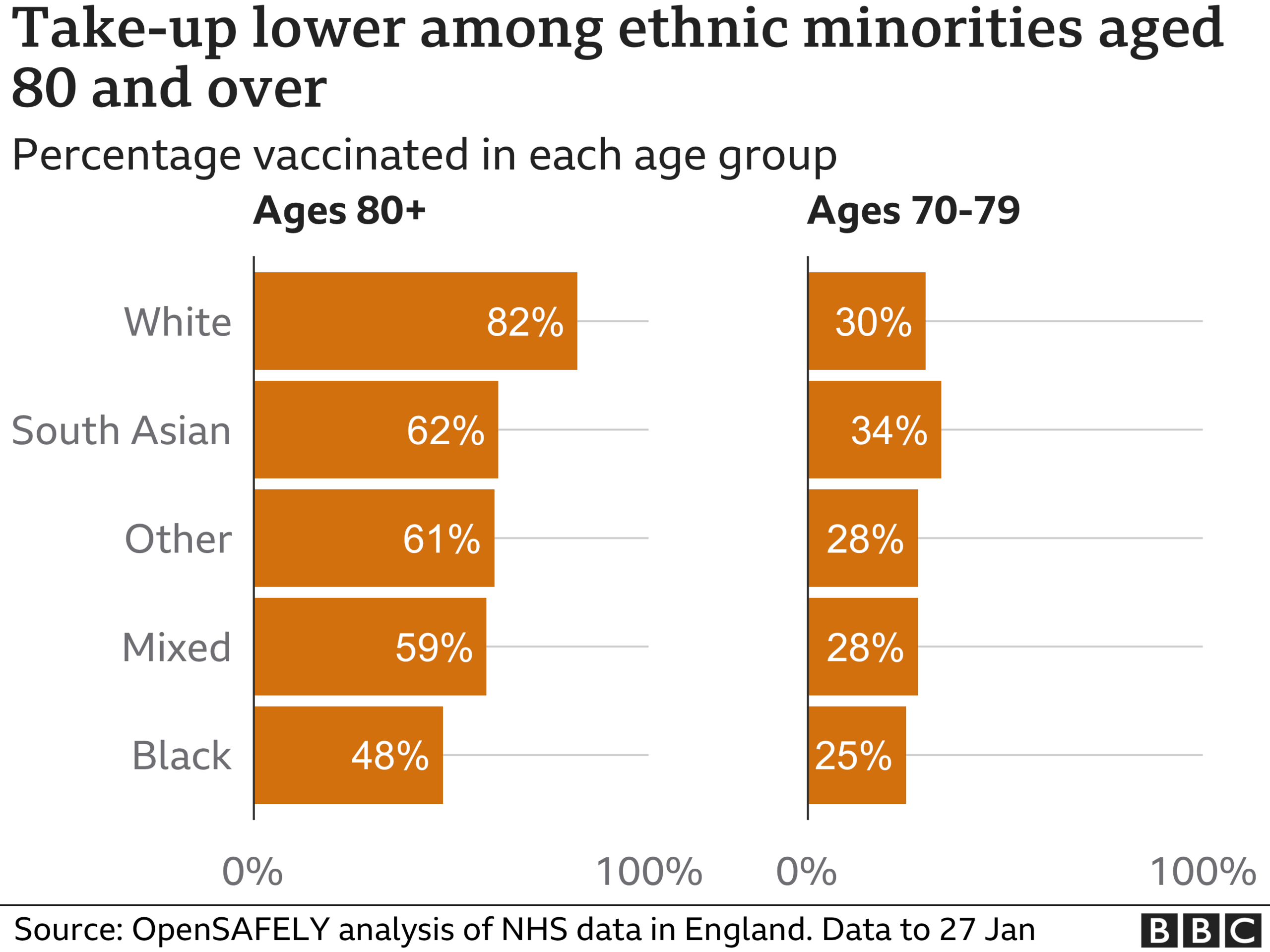
This OpenSafely analysis draws data from about 40% of GP practices.
There are official statistics of vaccine uptake, external which show how many people in each ethnic group have had the vaccine, but they are not broken down by age or location.
Normally we would look at how these compare with the overall size of the population, but we don't have much of an idea of how many people are in each ethnic group.
This is because the last census was done ten years ago.
Public Health England has said that, external supplying transparent data by ethnicity will "will help to build confidence in the fairness of offer - as will updates on the actions being taken to address inequalities in access or uptake that are identified."
2. How many staff in care homes have been vaccinated?
Care home staff were one of the first groups to be prioritised.
But there are no publicly available statistics of how many of England's 1.2m care staff have been vaccinated.
On 15 February, Health Secretary Matt Hancock indicated that around two-thirds of this group had received their first dose, including staff who deliver care in people's homes.
He also indicated that about 80% of England's two million NHS staff had received the vaccine.
In Scotland, external it is estimated that 91% of staff in care homes for the elderly are vaccinated and 83% in Wales, external.
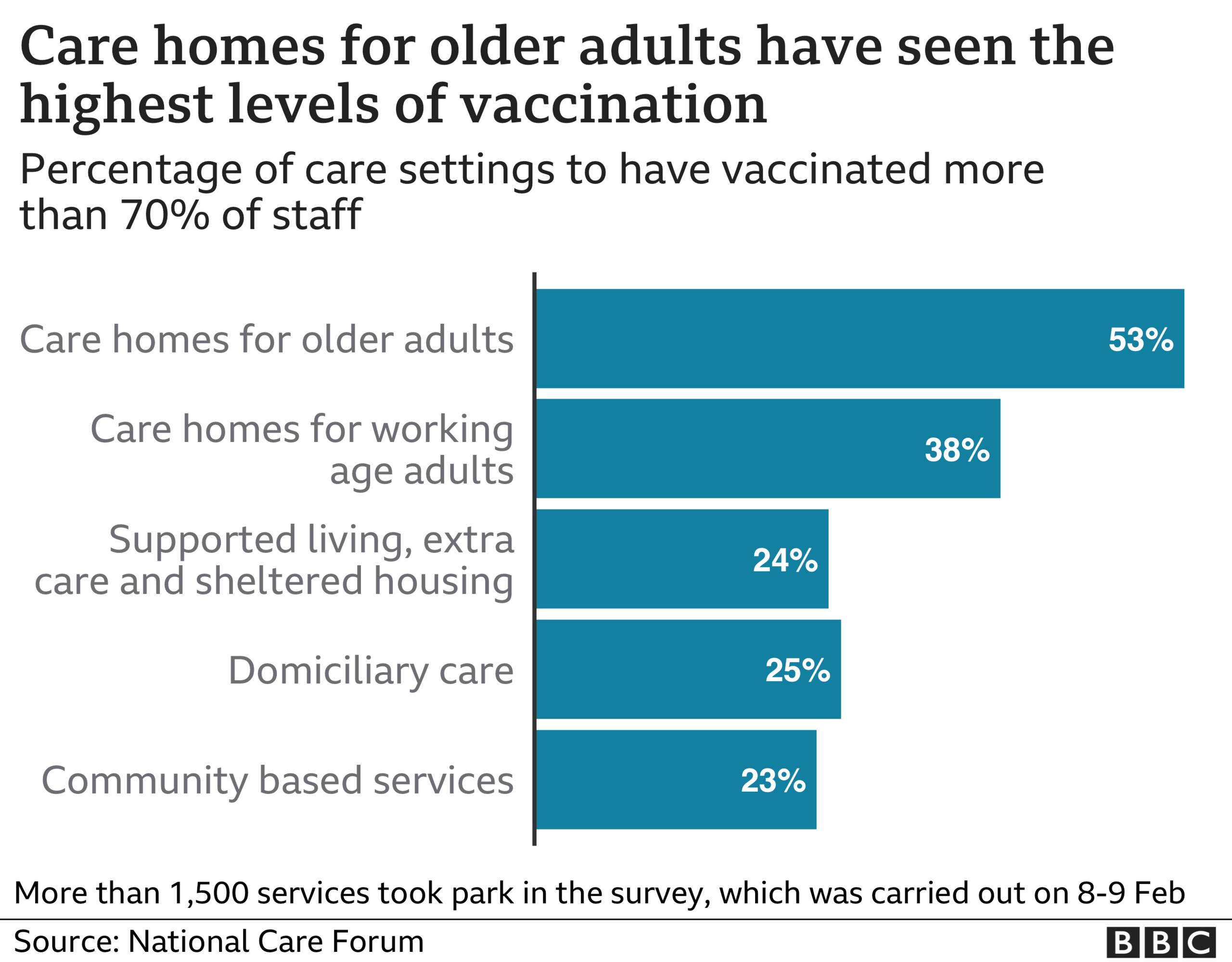
The National Care Forum, a body representing not-for-profit care homes across the UK, found that half of the homes for the elderly which were surveyed had had less than 70% of their staff vaccinated.
The survey, which was conducted on 8-9 February and reached around 1,500 care services, showed that the reason for not having the vaccine was split evenly between vaccine hesitancy, lack of access, waiting for an appointment and health reasons.
3. How do we know everyone was "offered" a vaccine?
The government said that the following groups should have been "offered" a vaccine by February 15:
Everyone aged 70 and over
Care home residents
Care and health staff
Clinically extremely vulnerable
Leaders have announced that this target has been hit in England, Scotland and Wales.
An "offer" means you've received an invitation for a vaccine, normally through a phone call, text or letter.
Currently, we have no data on how many people have actively turned down the offer of a vaccine or have ignored their invitation for a jab.
We also don't know how many of the 15m people vaccinated are outside of these priority groups.
These numbers would give a clearer picture on whether the target has been hit, and highlight where vaccine hesitancy is high.
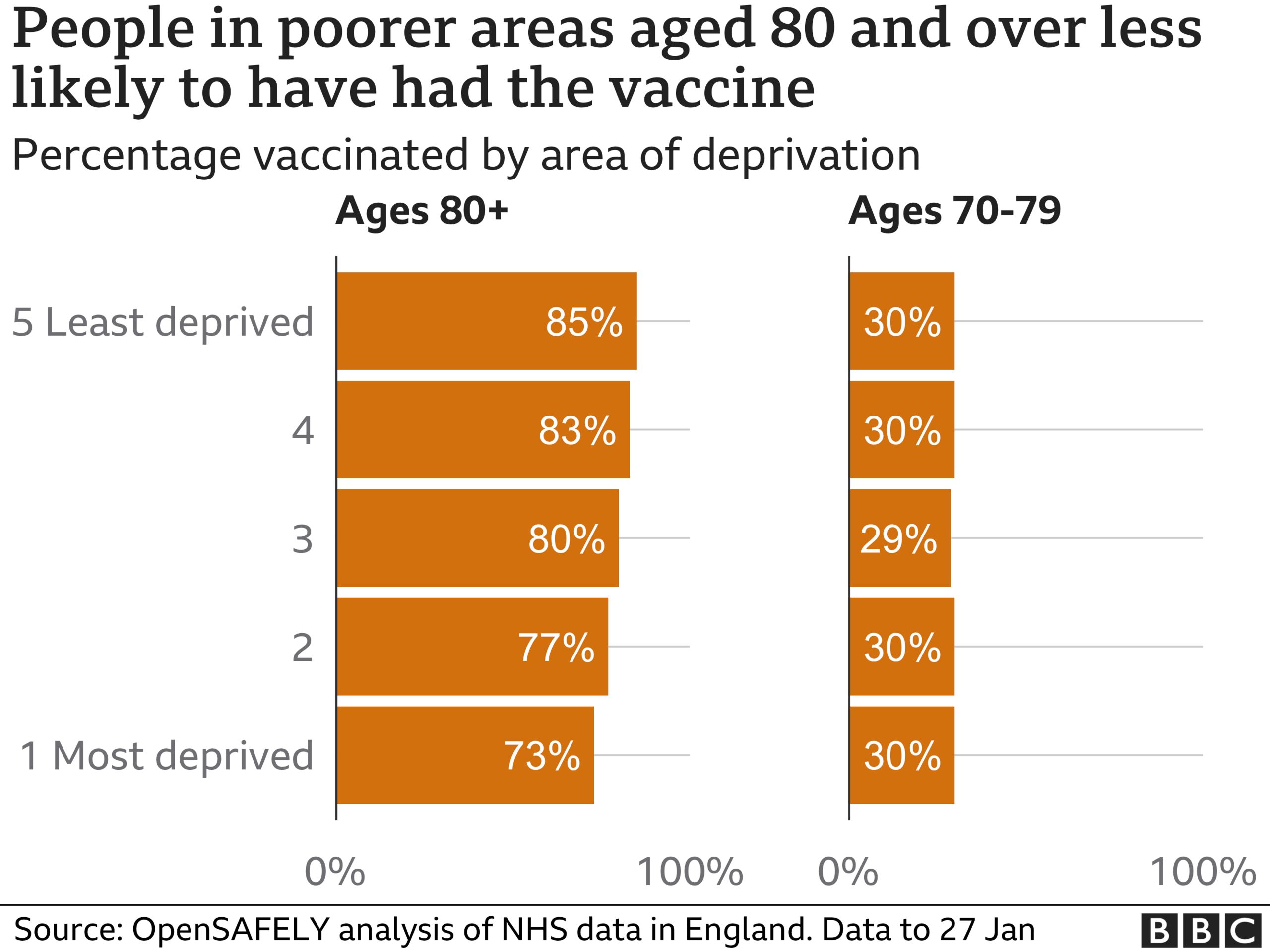
For example, data from OpenSafely shows vaccination uptake is higher in wealthier areas, but it doesn't highlight whether the apparent lower uptake in more deprived areas is down to people refusing a jab, or simply not communicating with the NHS.
The UK Statistics Authority, which regulates the government's use of statistics, external, requested this information (as well as data on ethnicity and care staff vaccinations) on 20 January.
4. Will we have enough supplies?
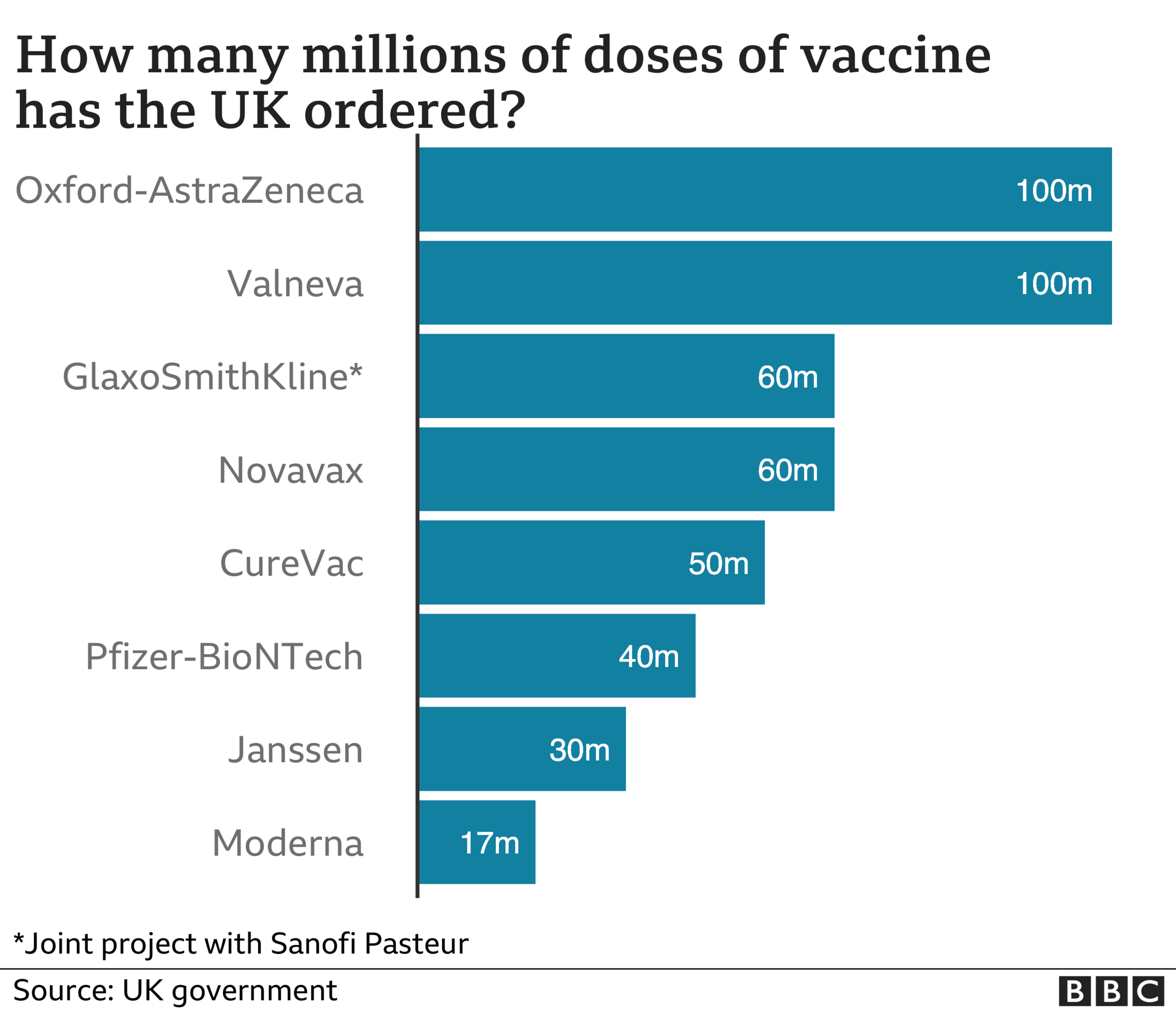
While we know the government has ordered enough vaccines overall, we do not know the details of when these will be delivered.
Health Secretary Matt Hancock has repeatedly said that supply is the "limiting factor" in the speed of the rollout.
The government expects to have enough supply to give people their second dose within three months, while also ensuring the next priority groups have their first dose.
People who have had their first dose have a considerable amount of protection from the virus, but the second dose increases this.
Getting the second dose within three months is not a rigidly set time-frame, says Eleanor Riley, a professor in immunology and infectious disease at the University of Edinburgh.
"The main concern is that if people miss this twelve-week window for the second dose, there is a danger that they fall out of the system and don't get their second dose at all. This would be very worrying, as the second dose is essential for conferring high levels of long-lasting immunity," she says.

Currently, just 4% of people who've had their first dose, have gone on to have their second.
This is because the health service has been focused on delivering the first dose.
5. Who will be vaccinated next?
Currently, the government has a list of nine groups who will be vaccinated before anyone else, including care staff, the clinically vulnerable and anyone over 50.
After that, the Joint Committee on Vaccination and Immunisation (JCVI) will make suggestions on the next priority groups for the government to consider.

In January, Vaccine Minister Nadhim Zahawi said that it's his "very strong instinct... to say, those who through no fault of their own other than their work, have to come into contact with the virus, should be prioritised".
He listed shopkeepers, teachers and police officers as those who might be prioritised next.
This piece has been updated to reflect increased orders of the Valneva and CureVac vaccines.


