Families back push to boost blood cancer treatment
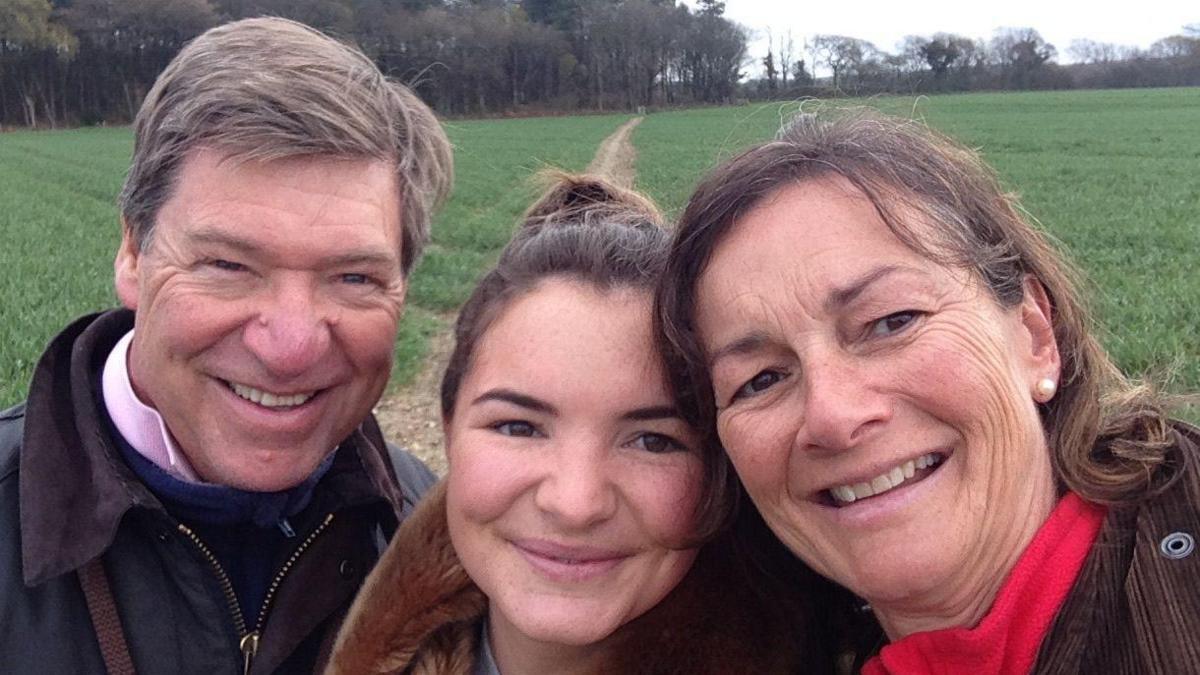
Nick and Katrina Bromfield with their daughter Zoë, who died in 2019
- Published
Patients and families in the south east are backing a campaign to improve how the NHS handles blood cancer cases.
Blood Cancer UK said the five-year survival rate for patients with cancers such a acute myeloid leukaemia (AML) and myeloma is less than 50%.
Working with patients and their families, the charity has drawn up an action plan to improve NHS specialist roles, boost diagnoses, remove barriers to care and drugs and enhance national data collection.
Nick and Katrina Bromfield, from Canterbury, Kent, whose daughter, Zoë, died from acute promyelocytic leukaemia, said: “We passionately believe that greater awareness and earlier identification are the key to improving the chances of surviving blood cancer."
Zoë was 26 when she died in 2019.
Her symptoms were initially misdiagnosed as tonsillitis, but two days later she suffered a brain haemorrhage caused by the blood cancer.
She spent 25 days in a coma in intensive care before she died.
The family said in a statement: "Her condition was not diagnosed until she was in hospital, by which time it was too late to save her."
Her parents said improving awareness and identification would spare other families from the trauma that they and Zoë's friends have experienced.

Gill Murphy underwent a stem cell transplant after a shock leukaemia diagnosis
Gill Murphy was diagnosed with acute lymphoblastic leukaemia (ALL) 10 years ago after initially dismissing her symptoms as tiredness from parenting a two-year-old.
Ms Murphy, who lives in Ashstead, Surrey, also noticed she was bruising easily and had two nosebleeds, which was unusual for her.
When she told her GP about her tiredness in passing, they ordered blood tests for her to check it wasn't anything sinister.
But when she was told to go to A&E, she knew something was very wrong.
Ms Murphy said: "I know very little about different types of cancers but I was thinking 'don't let it be anything that ends in -oma or - aemia'.
"And then [the doctor] walked in and told me I had acute leukaemia."
'Really fortunate'
ALL is common in children and older adults, but rare for people in their 40s like Ms Murphy was.
She was put on a national clinical trial which consisted aggressive chemotherapy and immunotherapy for near six weeks, as well as regular, painful bone marrow biopsies.
"I'm really, really fortunate to get into remission after the first stage," Ms Murphy said.
"With my type of blood cancer it can come back in a heartbeat, so you have to really keep knocking it on the head with different types of chemotherapy."
Following her treatment which included a stem cell transplant, Ms Murphy feels lucky to have had clinical nurse specialist and care while in remission.
She said: "Having that contact just made a huge difference and I know a lot of people don't get that."
'New research'
Blood Cancer UK says despite being the fifth most common cancer and the third biggest cancer killer in the UK, blood cancer does not receive the public profile of the other four common cancers.
It is marking the start of its annual Blood Cancer Awareness Month to urge people to write to their MP asking them to back its recommendations for improvement.
Its taskforce co-chair, Prof Adele Fielding, said: "The UK has started to fall behind the international standard in many and often very basic ways such as staffing levels, availability of new drugs and opening of new clinical trials.
"Coupled with a dwindling pipeline of UK clinical academics to conduct new research, I fear things may get worse."
Follow BBC South East on Facebook, external and on X, external. Send your story ideas to southeasttoday@bbc.co.uk, external or WhatsApp us on 08081 002250.
Related topics
Related internet links
- Published28 August 2024

- Published1 February 2024

- Published7 June 2024

- Published22 June 2024
