Old hospitals added to Covid infection spread risk
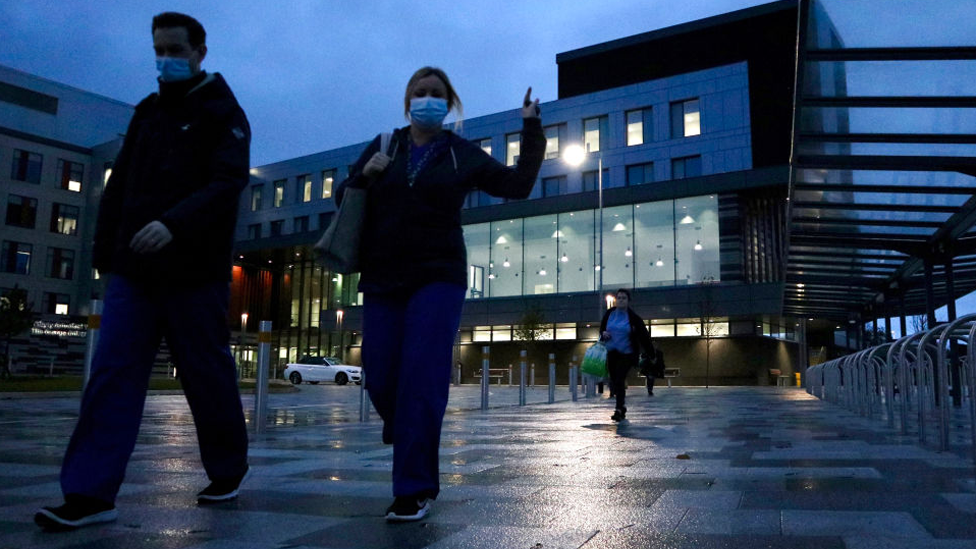
The new Grange Hospital at Cwmbran, which has single rooms, opened in November 2020, just before the second wave of the pandemic
- Published
Ageing hospitals and significant delays in discharging patients from hospital during the Covid-19 pandemic meant the NHS struggled to manage the risk of the virus spreading, a new report has found.
NHS Wales has been working with health boards to learn lessons from the cases of more than 18,350 patients who caught Covid while in hospital over a two-year period from March 2020.
Its final report also points to variable bereavement support available for families, while there were a number of instances when communication also fell short.
NHS Wales said it had identified areas for improvement which "remains a priority for all NHS organisations".
Public Health Wales had already estimated that 2,400 patients died within a month of catching Covid while in hospital, during the two-year period under examination.
However, these deaths are from all causes and it is not possible to say exactly how many died from Covid itself.
But the first wave of the pandemic saw a third of patients who caught Covid in hospital dying within a month.
NHS Wales' National Nosocomial Covid-19 programme, external has been looking at hundreds of cases investigated by health boards, although it insists it is separate from the UK Covid inquiry and was also not looking to place blame.
It has identified a number of challenges and recommends key learning points.
The pandemic highlighted the impact modern hospital design, such as the availability of single rooms, can have on strengthening infection control.
It found many older hospitals had limited availability to isolate patients so many patients faced multiple ward movements.
Families also found that they were often not informed of these movements, which resulted in additional difficulties when seeking updates.
Health officials said there were huge difficulties in stopping the spread of Covid in busy places like hospitals, which operated like small towns.
The NHS in Wales was recently estimated to have £793m maintenance backlog and nearly half of buildings are at least 40 years old.
But in the short term, managers were to look at opportunities to make better use of existing space.
Facing unprecedented pressure, the report found there was a worsening of delays to discharges of patients who were otherwise medically fit to leave hospital.
Delays meant an increased risk of deterioration and infection.
It also found:
Some poor experience of communication to families around patient updates, negatively impacted by sustained pressure on staff and visiting restrictions
Visiting restrictions themselves had "many adverse effects" on the physical and mental health of patients - "especially those in the vulnerable groups that the restrictions were intended to safeguard, many of whom were not able to fully understand the decisions made".
Some NHS organisations did not have dedicated bereavement support until a national framework was set up in 2021. This came too late for some families
Ongoing issues with staff recruitment. Gaps in vacancies had exacerbated pressures and despite best efforts, patient care was at times compromised
What is happening with Covid now?
Public Health Wales is still recording patients who are catching Covid while in hospital. There have been more than 2,380 hospital-acquired infections so far this year
Surveillance of Covid in the community suggests infections rise and fall during the year - and do not behave seasonally like flu
Infections are currently falling again after peaking in late July
Random samples of hundreds of patients attending hospitals in Wales showed around 10% testing positive for Covid, in the most recent week
Most of the current Covid cases being tested in Wales since June have been the KP.1, KP.2 and lately the KP.3 or FLuQE sub-variants of Omicron
There have been 285 deaths due to Covid so far this year - 56% of the levels we saw in the same period last year and 31% of the mortality in 2022
What has been the response?
The programme's interim report last year dealt with the issue of "do not resuscitate" notices and these are highlighted again.
Families early in the pandemic raised concerns there was a "blanket approach" to applying the decision when somebody was diagnosed with Covid.
The review found there was no evidence that decisions had been made inappropriately or against policy, however improvements in how they were communicated to patients and families were needed.
The findings also pointed to some patient note-taking not being up to standard but it acknowledged "extreme system pressures" facing staff at the time.
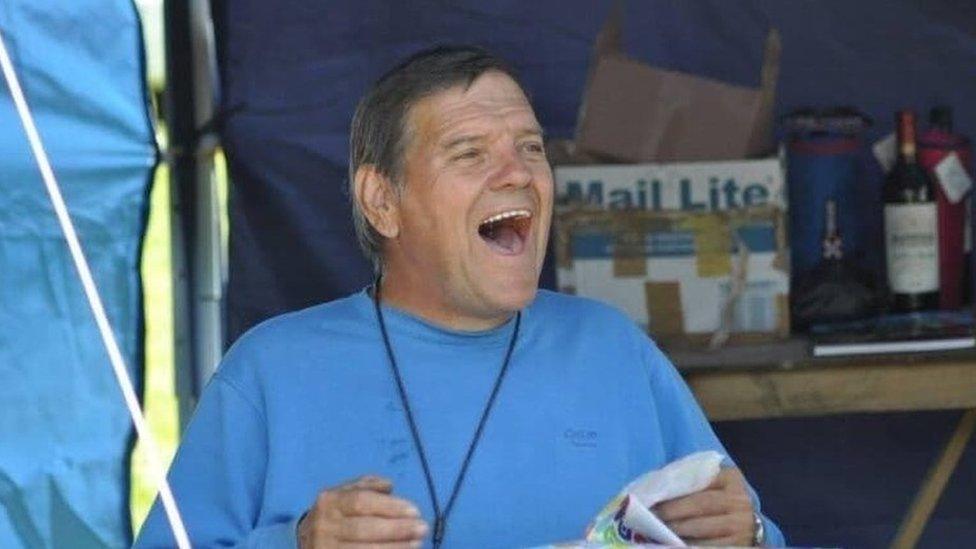
Jennifer Winslade, executive director of nursing at Aneurin Bevan health board, speaking on behalf of NHS Wales, offered her sincere condolences to all those who lost loved ones after acquiring Covid-19 in healthcare settings, saying "the impact cannot be underestimated".
"Developing our understanding about nosocomial Covid-19 and people's experiences will have a lasting impact on improving the quality of healthcare services we provide in Wales."
Prof Pushpinder Mangat, deputy chief medical officer, said they were looking at more consistency across the health service.
"I don't think we can prevent those things [pandemics] but should it happen again, I think we are in a better position to cope," he said.
Health Secretary Mark Drakeford said he was committed to ensuring the findings would lead to "meaningful change" and improvements in the quality and safety of patient care.
"I would like to thank all the individuals and organisations across the NHS in Wales for their commitment and dedication to this challenging work," he said.
"I also pay tribute to, and thank, all the families who lost loved ones for their patience as we have worked to find answers for them."
Conservative health spokesman Sam Rowlands called on the NHS to be modernised.
“Many of the recommendations in this report marry up with Welsh Conservative calls that Labour have so far ignored, from the need for NHS staffing investment, ending discharge delays and digitalising record keeping," he said.
Related topics
- Published28 May 2024
- Published19 September 2019

- Published10 December 2020