'People are dying because they're not getting care'
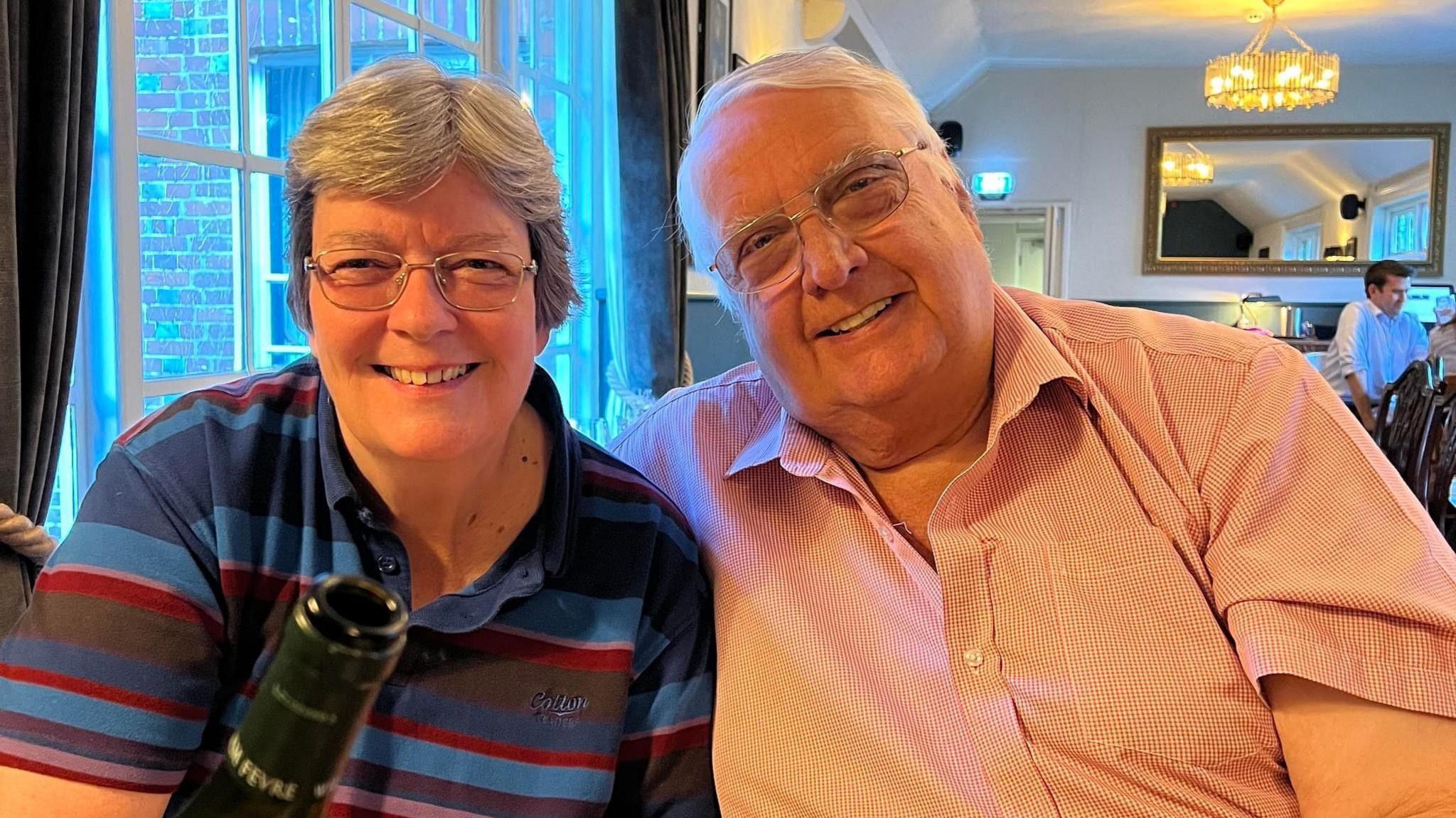
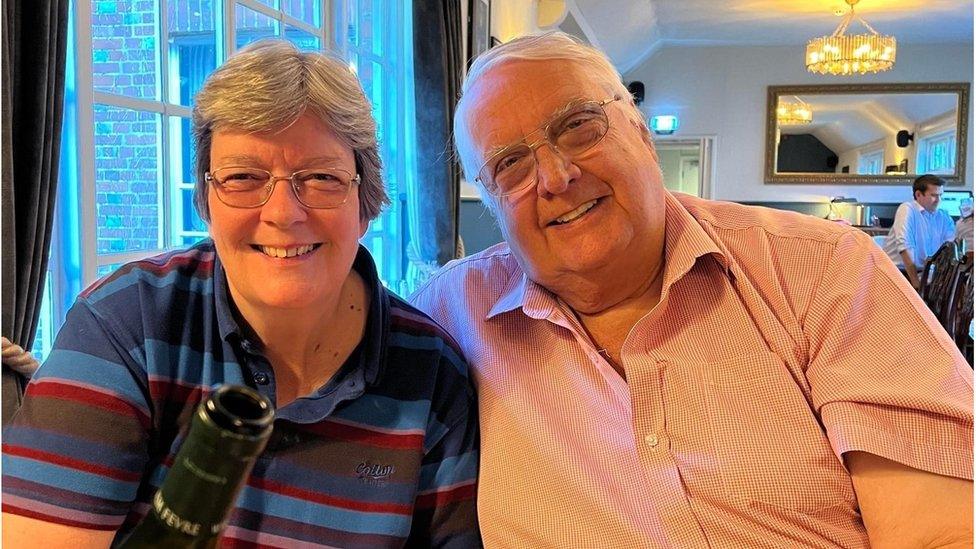
Tony Hudson, pictured with wife Di Hudson, died following a suspected stroke in December 2022
- Published
Three hospitals in Devon and Cornwall have the poorest record for ambulance handover delays in England, with the highest proportion of patients waiting longer than an hour, according to BBC analysis of NHS data.
The analysis showed Derriford Hospital, Royal Cornwall Hospital and Torbay Hospital each had more than 40% of patients arriving by ambulance waiting for longer than 60 minutes to be handed over to A&E staff last winter, compared with a national figure of 8.8%.
Di Hudson, from Bodmin, whose husband Tony died from a suspected stroke after a 13-hour wait for an ambulance, said the figures were "really worrying".
The NHS apologised and said it was working hard to improve wait times.

The NHS in Devon and Cornwall have both apologised for the delays
The BBC analysed daily handover statistics published by the NHS between November 2023 and March 2024.
The analysis showed 63% of patients who arrived by ambulance were left waiting in the ambulance for more than 60 minutes at Derriford Hospital in Plymouth over that period.
It showed 55% of patients waited longer than an hour at Royal Cornwall Hospital, while 45% of patients waited longer than an hour at Torbay Hospital.
The national target is for all handovers between ambulances and emergency departments to take place within 15 minutes, with no-one waiting more than 30 minutes.
Tony Hudson, 74, died at Royal Cornwall Hospital on 27 December 2022.
Mrs Hudson said she called emergency services at about 01:00 on December 15 2022, but the ambulance arrived after 14:00 the following day.

Mrs Hudson said the situation was "terribly, terribly serious"
She said she was not surprised hospitals in Devon and Cornwall were at the bottom of the league table.
“As I said last year, it always worried us there was just one hospital in Cornwall," she said.
"I don’t know whether anybody really realises how terribly, terribly serious this is.
"I mean, people are dying because they're not reaching emergency care."
'Our hospitals are full'
Dr Ian Higginson, vice president at the Royal College of Emergency Medicine, said "emergency care is in a mess at the moment".
"Both patients and staff will tell you that," he said.
"The major problem we face is overcrowding in our emergency departments, and that's because our hospitals are full.
"And then we might see patients in our corridors or even our car parks stuck in ambulances."

“Emergency care is in a mess at the moment," said Dr Ian Higginson
He said the South West was not unique but the region did have some specific challenges.
“We do have an elderly population, pockets of deprivation," he said.
"Some areas where they aren't enough GPs.
"We can also at times be quite a rural area, and there is of course seasonal variation for some areas."
Dr Higginson said he was disappointed emergency care was not a "hot topic" during the election campaign.
"Most of the manifestos were pretty light on detail regarding how the parties were proposing to fix urgent and emergency care," he said.
"It would be good to see it higher up on the political agenda."
'Very sorry'
Two of the three hospitals responded to the BBC's request for comment.
Both acknowledged patients faced "unacceptable waiting times in ambulances".
University Hospitals Plymouth NHS Trust said: "We are very sorry to anyone who experiences these waits.
"We are working hard to ensure people are treated in a timely way, and from March 2024 to May 2024 we recorded a reduction in around 3,000 hours of ambulance hours lost to delays.
"However, we know there is still significant work to do."
NHS Cornwall and Isles of Scilly said: "We are sorry that patients wait for longer than they should to be seen within the emergency department and are working across the health and care system to address this as one of our highest shared priorities.”

How will the parties tackle healthcare problems?
The Conservative Party said it would recruit 28,000 doctors and 92,000 nurses by 2029.
It said it would build 40 hospitals by 2030, have 250 new and modernised GP surgeries and create 50 community diagnostic centres, invest £3.4bn in paperwork-cutting tech for doctors and nurses, increase NHS spending above inflation every year and create 2.5 million more NHS dental appointments by reforming the dental contract.
The Green Party said it would improve NHS staff retention and cut waiting lists by raising pay (including 35% for doctors) and increasing NHS funding by £8bn a year plus £20bn for hospital buildings.
It said it would also guarantee patients rapid access to GPs and access to NHS dentists, allow access to evidence-based mental health therapies within 28 days and support a law change on assisted dying for the terminally ill.
The Labour Party said it would end "the 8am scramble" for GP appointments, train more GPs and guarantee face-to-face consultations.
It said it would pay NHS staff extra to work evenings and weekends enabling 40,000 more appointments a week, create thousands of medical training places, modernise NHS buildings and equipment to catch conditions earlier, provide 700,000 more NHS dentistry appointments a year and recruit 8,500 mental health staff.
The Liberal Democrats said it would guarantee GP appointments within seven days, and 24 hours if urgent, and attract 8,000 more GPs and have walk-in mental health hubs for children and young people.
It also said it would guarantee NHS dentist access for urgent and emergency care, and launch a 10-year plan to invest in and repair hospitals.
Reform UK said it would cut NHS waiting lists to zero, boost recruitment by letting staff work for three years tax-free, end staff training caps and use more independent providers.
It said it would let patients go private if treatment deadlines were missed, offer 20% tax relief on private healthcare and insurance to encourage non-NHS treatment and hold a public inquiry into excess deaths and vaccines.
Follow BBC Cornwall on X (formerly Twitter), external, Facebook, external and Instagram, external. Follow BBC Devon on X (formerly Twitter), external, Facebook, external and Instagram, external. Send your story ideas to spotlight@bbc.co.uk, external.
- Published13 January 2023
- Published5 January 2024
