'I've a new lease of life thanks to respiratory hub'
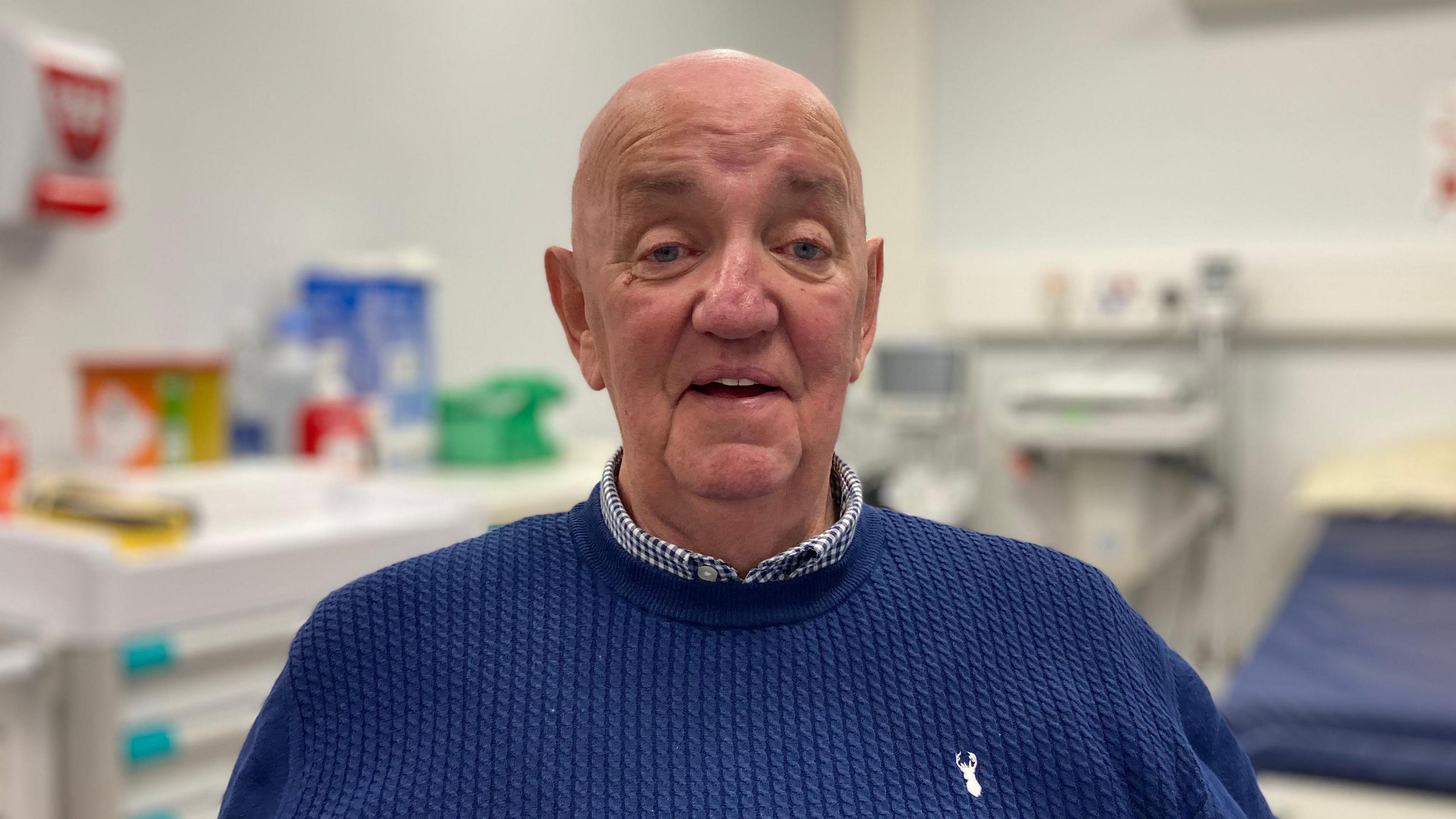
Jim Ross said the hub at Altnagelvin has given him "a second chance of life"
- Published
A man has praised Altnagelvin Hospital's respiratory hub for giving him "a second chance of life".
Jim Ross, from Londonderry, was admitted to hospital after fluid was found in his lungs following a fall in December 2022.
The 75-year-old had been "convinced" he had asbestosis, external because of working in a power station for more than 30 years.
But after almost two years of tests and treatment, he has just got news that has "given me back my life and the family's life".
"It wasn't until a few days ago that they said 'we're convinced you don't have asbestosis or lung cancer'," he said.
"I could have cried. I was just overwhelmed. I really was. I still at times give myself a shake."

Jim Ross with his wife Lorna and his daughter Gayle
Jim has described his care at Altnagelvin's respiratory hub as "lifechanging" and is now looking forward to Christmas and planning future family holidays.
This was something he had been afraid to think about until last week.
"It hasn't been easy," he said, but he managed with great family support.
What is respiratory disease?
Respiratory disease, external is a wide set of conditions that affect people's lungs and therefore affect their ability to breathe properly.
It includes conditions such as asthma, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, asbestosis and lung cancer.
According to one charity, external, respiratory disease is "one of the top three killers in Northern Ireland", with one in five people being diagnosed with a lung condition at some point in their lives.
The hub at Altnagelvin Hospital secured permanent funding a year ago.
While only operating two and a half days a week, the Western Trust said it is keeping a significant number of patients out of hospital and saving a significant number of beds.
It said 1,321 patients were seen between April 2023 and April 2024, with about half (684) of them in the Emergency Department (ED).
About a sixth of those, 223 patients, have avoided being admitted to hospital, saving more than 300 hospital beds.
The trust said 53% of patients admitted to the respiratory ward are over 70.
'One-stop shop'

Dr Paddy McShane said respiratory disease puts pressure on the health service particularly in the winter
Paddy McShane, a specialist respiratory doctor, said the hub is helping with patient flow through the hospital.
He said the hub is a "one-stop shop" for those with suspected or confirmed respiratory illnesses.
Patients can been seen by a senior respiratory doctor, have diagnostic tests, get results immediately and start the appropriate treatment without needing a second visit.
"We would see 120 to 130 patients every month in the hub that are patients who would have stayed in hospital for longer periods of time," Dr McShane said.
"It's freeing up turnover and getting more people out of A&E."
How does it work?
Dr McShane explained how a respiratory consultant will make assessments on patients in the Emergency Department every morning.
Some of these patients, who have come in overnight, may not need to be admitted to hospital, but cannot wait six weeks for an outpatient appointment.
However, now patients can be sent home with treatment and will have a follow up at the hub several days later to ensure they have not deteriorated.
"We decrease the number of patients in A&E, but we've got the backup that we know they're going to be seen within 24 to 48 hours in the respiratory hub," Dr McShane said.
Winter pressures
He added that respiratory disease puts pressure on the health service all year round but particularly in the winter.
"We have a lot of winter viruses and bacteria that cause infections, and people with underlying respiratory disease are more susceptible to developing these infections," he said.
"Our A&E departments are full now.
"There's people that are very unwell, very breathless, very sick with infection, and it's not ideal, but at the minute we have to work with what we've got," he said.

The hub's team has received "very positive feedback" from patients such as Jim Ross
Dr McShane said the hub also helps the hospital's main respiratory ward with consultants being able to discharge patients earlier freeing up beds.
"Needing to be in hospital is one thing but staying in hospital for a prolonged period of time, particularly over the winter, in wards that everybody's got a different bug [is another].
"It's protective to try to get our patients home, and we know that they do much better at home, and they want to be at home."
Dr McShane said the hub is "definitely working" and the team has received "very positive feedback" but they would like to see the service expanded.
"There's a need for it at the weekend too, not just a Monday to Friday, but like all of the health service everyone's looking for more money, and every specialty could do with a lot more.
"But we also understand that the public purse isn't overflowing," he added.
The Department of Health said work is ongoing to develop a regional lung health plan.
But that "while the minister will continue to make the case for greater resources for health, the absence of adequate funding will continue to impact the pace of implementation".