HIV-positive woman calls for IVF change in Ireland

Ainara and Peter are getting IVF treatment in Spain
- Published
A woman living with HIV says she has been unable to access publicly funded IVF treatment in Ireland due to a lack of laboratory facilities.
Ireland introduced free fertility treatment for eligible patients in 2023 including some treatments for people living with HIV.
But currently, there are no labs that can provide services for HIV-positive women who require IVF as legally there must be separate storage facilities for their samples.
The Irish government said it was planning to open a new fertility centre in 2025 “with a view to developing a public service inclusive of... IVF [and other treatments] that can treat and care for individuals living with HIV positive".
The Health Service Executive (HSE), which runs public healthcare in Ireland, told BBC News NI that advances in HIV treatment mean it is working to review its practices.
It said some laboratories elsewhere had started using "effective scheduling and cleaning" - not necessarily separate lab areas - to "mitigate risk related to any potential cross-contamination of samples".
With HIV 'the doors start closing'

Ainara and Peter need fertility treatment to have a baby
Like thousands of people in Ireland, Ainara Pederoso and her husband Peter plan on having a family.
After moving to Cork and marrying, the couple began trying for a baby.
When they were not successful, they had tests and it became clear because of an underlying issue with Peter’s fertility, they would need IVF treatment.
Ainara, who is from the Canary Islands, said she contracted HIV from a previous sexual partner and was diagnosed in 2017.
She said the virus had been detected early and was "undetectable" in a matter of months.
Undetectable, according to HIV services, means that the risk of the virus being transmitted to a partner through sex or to a foetus is zero because the level of the virus – known as viral load – is so low.
'Sorry, but we won't be treating you'
Ainara said she found it hard to get answers to questions about accessing fertility treatment.
“When I told them I had HIV is when all the doors start closing," she said.
“We know that in the UK, people with HIV can get on the government scheme.”
In Northern Ireland and other UK regions, eligible patients who live with HIV can access fertility treatments including IVF - in which eggs are removed from ovaries and fertilised with a partner's sperm or a donor's sperm in a laboratory.
They contacted private IVF providers but none could facilitate them.
Ainara has begun a petition to highlight the need for public lab facilities in Ireland.
“I know that this is not going to benefit me. I'm not doing this for pity.
“I was ready for hate because of the stigma, but someone has to speak about this.
"Everyone said: ‘We didn't know about this. You were so brave. Thank you for speaking about us.’
“Many people have said they had to go abroad and adopt, or just gave up because they can't afford adoption, or afford a fertility treatment.”
Ainara hopes to influence change by speaking publicly.
“The first impression after my diagnosis was not thinking about having a child or getting a family, it was the fear of having to say this to my parents, and I hid it for two years,” she said.
“I've noticed since I started the petition, women contacting me and saying: ‘Please don't say my name, because many people in my family don't know, or I just want to so support you, but please don't share my message.’
“So a lot of women out there with HIV are scared because of the stigma and how people around them are going to react if they break the news, which is a shame, because indeed, we have kind of normalized that HIV is out there."
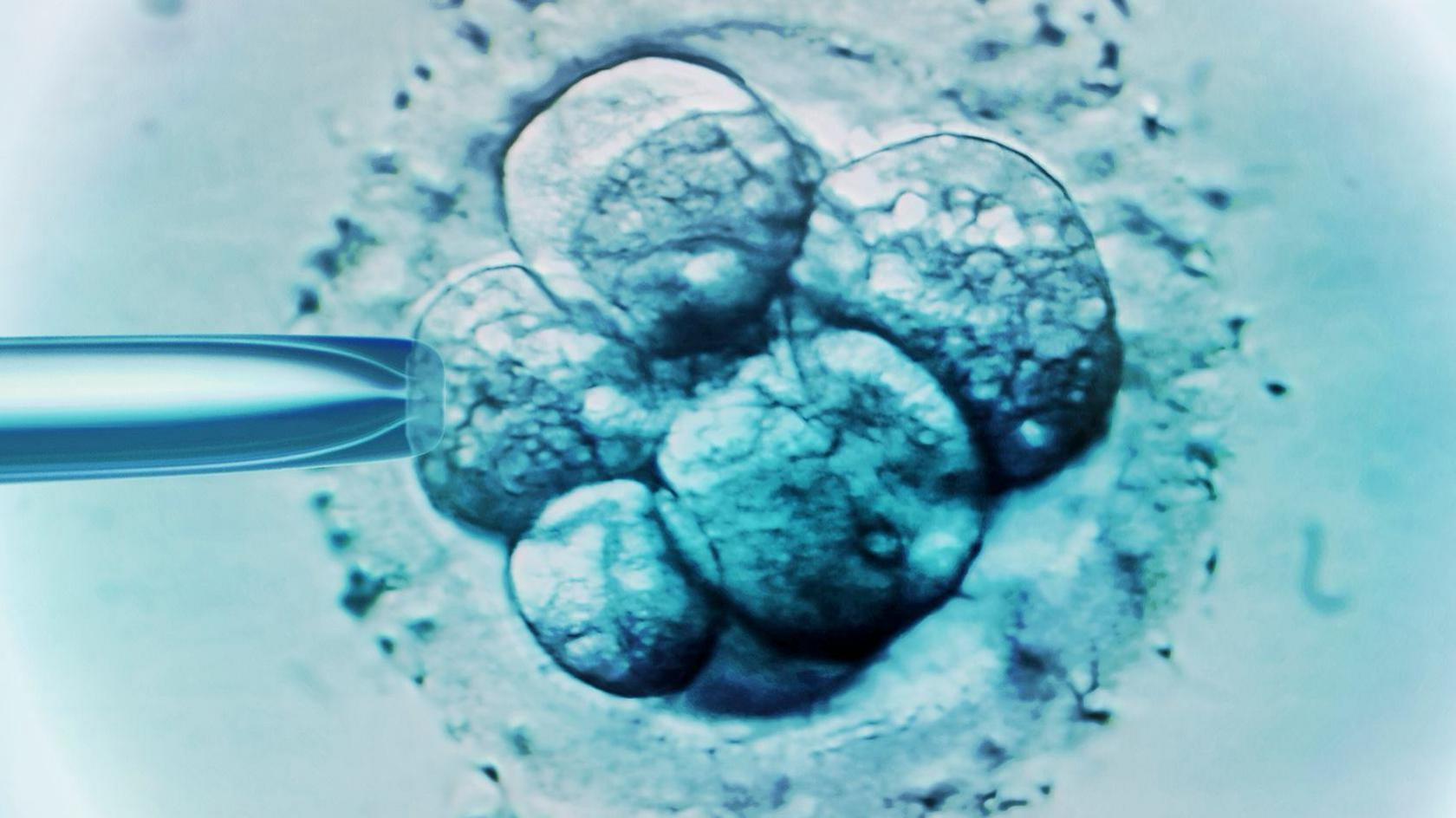
IVF involves removing eggs from ovaries and fertilising with a partner's sperm or a donor's sperm in a laboratory
High rates of HIV in Ireland
Official figures show Ireland has one of the highest rates of HIV, external in western Europe.
From 2019 to 2022, there was an increase in the overall number of diagnoses from 11.1 cases per 100,000 people to 17.2 cases per 100,000.
Two-thirds of Ireland’s HIV diagnoses in 2022 were among men while the rate of women being diagnosed doubled.
The Health Protection Surveillance Centre, external monitors transmissible diseases and largely attributes the changes to an increase in people with a previous HIV diagnosis made outside Ireland and migration.
The HSE told BBC News NI the government is planning to open a new national public fertility centre in Cork in 2025 “with a view to developing a public service inclusive of... IVF [and other treatments] that can treat and care for individuals living with HIV positive".
Regarding IVF, it said “no private provider in Ireland is currently positioned to offer care if either the female or the male is HIV+”.
At present, the statement said: “It is important to note that no patient living with HIV is being denied treatment” because eligible patients can get funding for treatment abroad."
Ainara said she and Peter did not appear to meet the requirements for publicly funded treatment abroad.
They are paying for IVF treatment in Spain.

What is HIV?
Human Immunodeficiency Virus (HIV) is a virus that attacks and destroys the body's T lymphocytes, a type of white blood cell, the reduction of which can then lead to the development of Acquired Immune Deficiency Syndrome (AIDS).
The infection is transmitted by body fluids, often during unprotected sex, but also through injecting drugs using unsterilised needles.
Individuals with AIDS have a weakened immune system and so are more vulnerable to opportunistic infections.
Currently, people living with HIV are given antiretroviral drugs which work by stopping the virus replicating in the body.
Related topics
- Published15 May 2024

- Published28 November 2022
