I felt like I was getting electric shocks - then found out it was cancer

Carol McGachie has been left with a permanent feeling that her finger tips are burnt
- Published
Every night when Carol McGachie went to bed she felt like she was being hit by electric shocks.
She would pace up and down while intense tingling pains went up her legs and down her arms.
The mother-of-two from West Lothian couldn't sleep a wink with the pain.
When she went to the doctor she was given painkillers for her sore back - but Carol thought there must be something more seriously wrong.
"I felt like I had been plugged into the mains," the 56-year-old told BBC Scotland News.
"It's an intense tingling that won't go away. You can't feel your skin or your hands properly.
"It's worse than pins and needles but on a similar vibe and a lot more painful."

Carol (front row second from right) said her family was keeping her mind off her illness
Carol felt scared and panicky when it then started happening in the daytime as well.
So she went back to the doctor and after almost a year of tests and scans she was diagnosed with myeloma, an incurable blood cancer.
Carol had six months of chemotherapy at the Western General Hospital from October 2022 and is now in remission.
"You do feel sorry for yourself in the beginning," she said.
"I know it's incurable and it will come back.
"Every time you get aches and pains you think, 'Is it back?' It is a bit of a nightmare."

Carol says having fun with her husband Michael is what gets her through her disease
So she now wants to live for the moment and to try to put it out of her mind.
"Sometimes it feels like you live from test results to test results every three months," she said.
"I know it's always going to be there and I don't block it out, but I try to move on a bit and it's not my central focus anymore.
"Having fun with my husband Michael really helps keep it off my mind. He is fantastic."
She is planning a lot more travel - she is going to Canada to visit her son, Ross, and her daughter Emma is getting married later in the year.
Carol, who also has two step-children, now has medication for the nerve pain, which helps to stop the feeling that she is being shocked.

Carol with her four children
"I'm still aware of it in the tips of my fingers and toes but it doesn't go up my legs and down my arms now.
"If I'm not feeling well or if I have a virus or a cold it comes back a bit.
"It feels like I have burnt fingers, I have that permanently all the time now."
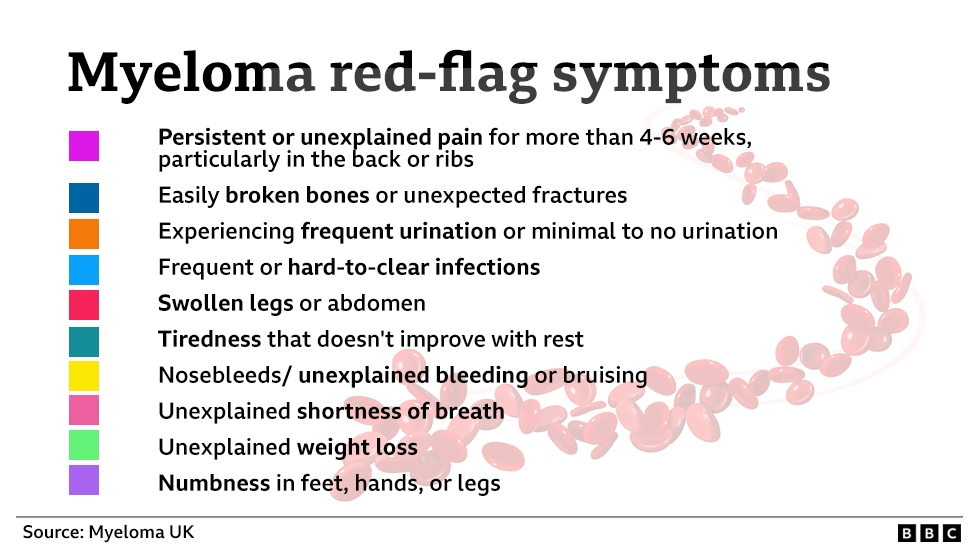
Dr Sophie Castell, chief executive at Myeloma UK, said that despite being the third most common type of blood cancer, myeloma was frequently missed.
That is because its symptoms, including back pain, easily broken bones, fatigue and recurring infection, are vague and often linked to general ageing or minor conditions.
"Every day counts while you're waiting for a diagnosis, and yet a third of patients visit their GP at least three times before being diagnosed," she said.
"One of the biggest barriers remains identifying the symptoms quickly and before too much damage is done.
"We know that doctors and patients can use very different language to describe the same symptoms."
She said they had now set up a symptom translator online, external in a bid to help doctors and patients catch the disease earlier.
Carol said: "I'm not sure why it took so long to get diagnosed but thankfully they found it before I had any organ damage.
"My advice would be: You know your own body so be more vocal and push a bit more with the doctor, rather than accept their word that it's nothing to worry about.
"You have to trust your instincts and not be embarrassed to keep going back to the doctor."
She enouraged doctors to ask for a blood test if a patient comes in with similar symptoms.
"I read something the other day that said myeloma is so rare that you have to be thinking about that when you see a patient just to rule it out," she added.
"Now I have it, I think my GPs are well on it."