Minor injuries unit staff say work is unsafe

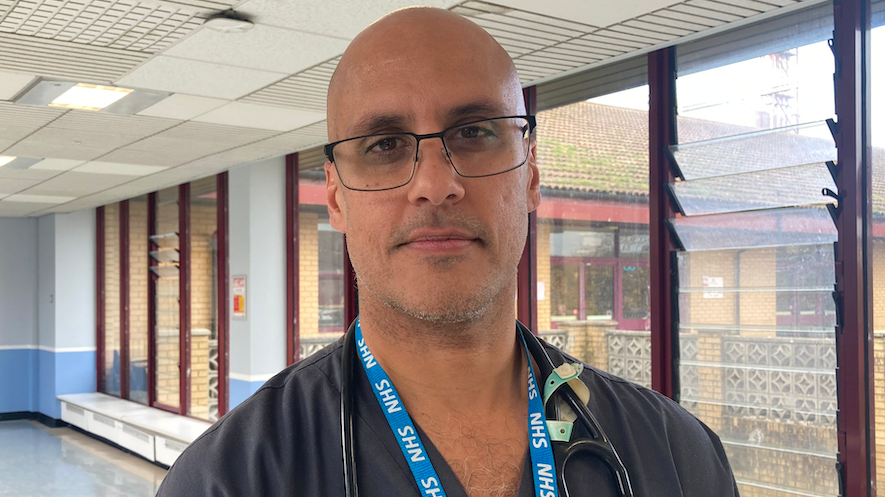
Dr Jon Morris says Hywel Dda health board is struggling to recruit staff to the unit
- Published
A GP at a minor injuries unit facing service cuts due to staff shortages has said work can feel "demoralising and unsafe".
The unit at Prince Philip Hospital in Llanelli, Carmarthenshire, treats patients with less severe injuries after its accident and emergency unit closed in 2016.
The decision to shut the unit overnight for six months from November has been widely criticised, prompting fears people could die.
Medical Director at the hospital Dr Robin Ghosal said Hywel Dda health board has unsuccessfully tried to recruit GPs "from within and abroad".
He said the plan to close between 20:00 and 08:00 from next month was temporary and aimed to keep staff and patients safe.
Clinical lead and GP at the hospital, Dr Jon Morris, said he often left work anxious.
"The worst-case scenarios are when we have surgical emergencies, unwell children, complications with pregnancy, because we’re not cut out to do that kind of stuff here," he added.
"It can be demoralising. At times it can feel very unsafe and quite upsetting at the moment."
Labour politicians attack injury unit cuts
- Published1 October 2024
Fears people could die as minor injury service cut
- Published11 October 2024
He said the minor injuries unit (MIU) had regularly become nurse-led overnight because doctors were unavailable.
"We have recruited 15 doctors over the last 12-month period, however, often, they come to the unit and see how it’s functioning and they then don’t want to take up shifts," he added.
Claire Thomas has nursed at the hospital for 25 years and sometimes feels scared at work.
“When you start to see the major stuff coming in, like last week we had six patients with chest pains within a half-an-hour time frame, that’s when you start to worry,” she said.
Even though minor injuries units are not designed to deal with life-threatening injuries, people have turned up needing urgent care.
The health board has urged patients in need of urgent or more complex treatment to go to the nearest A&E at Glangwili Hospital in Carmarthen or Morriston Hospital in Swansea.

Kay Rickett, 62, is worried about the temporary overnight closure of her local minor injuries unit
Kay Rickett, 62 from Kidwelly, Carmarthenshire, rushed to the unit on Monday after feeling excruciating pain in her knee while at a bingo session in Swansea.
She said she was told an ambulance would take eight hours to arrive and was advised by a paramedic to go to the MIU for an X-ray.
She called the overnight closure "appalling" and "the wrong decision", adding people without cars would not be able to get to Swansea or Carmarthen.
Protesters have set up a 24-hour camp outside the hospital site, urging the health board to reconsider the temporary plan.
"If someone’s sick, they need somewhere to go, especially if they’re badly hurt or injured," said councillor Suzy Curry.
"This MIU has saved people’s lives very recently."
Medical Director Dr Robin Ghosal said “Lots of innovative ways have been used to try and recruit both from within and abroad.
Dr Ghosal said the decision to pilot the closure of the unit overnight had "not been taken lightly".
He added: "But it’s an environment which, quite frankly, would be a very dangerous environment and that’s why we’ve made that difficult decision. It’s for everyone’s safety."
Analysis by Owain Clarke, BBC Wales health correspondent
This is clear evidence of the impact of staff shortages on yet another part of the Welsh NHS.
The MIU sees about 31,000 patients a year is led by GPs and nurses, but the health board argues that a lack of doctors has meant about 42 shifts couldn't be filled between February and July.
It's true that Hywel Dda health board has some the worst staff shortages in Wales, with vacancy rates for doctors and dentists reaching almost 20% and a number of surgeries also closing their doors.
But this isn't new.
Back in 2011, when the plans were announced to change the A&E at Prince Phillip into a Minor Injuries Unit, bosses argued then that services were spread too thinly.
For years they've promised that centralising services, including at a new hospital, would help with recruitment and put things on a firmer footing... but that hospital is still years from being delivered.
As challenges persist, people might feel angry about what they see as services being eroded with little to show in return.
The health board argues that safety of patients and staff lies at the heart of its decision, but cutting this service could increase the strain on neighbouring A&Es, at a time when those departments are bracing themselves for the most difficult months of winter.