How has coronavirus affected mental health?
- Published

The coronavirus pandemic has led to concerns about a worsening of mental health across the UK but what's the scale of the problem?
How has mental health changed?
Mental health problems have worsened across all age-groups in the past year.
In adults, the proportion of individuals showing symptoms of depression, external has almost doubled since the start of the pandemic, according to the Office for National Statistics.
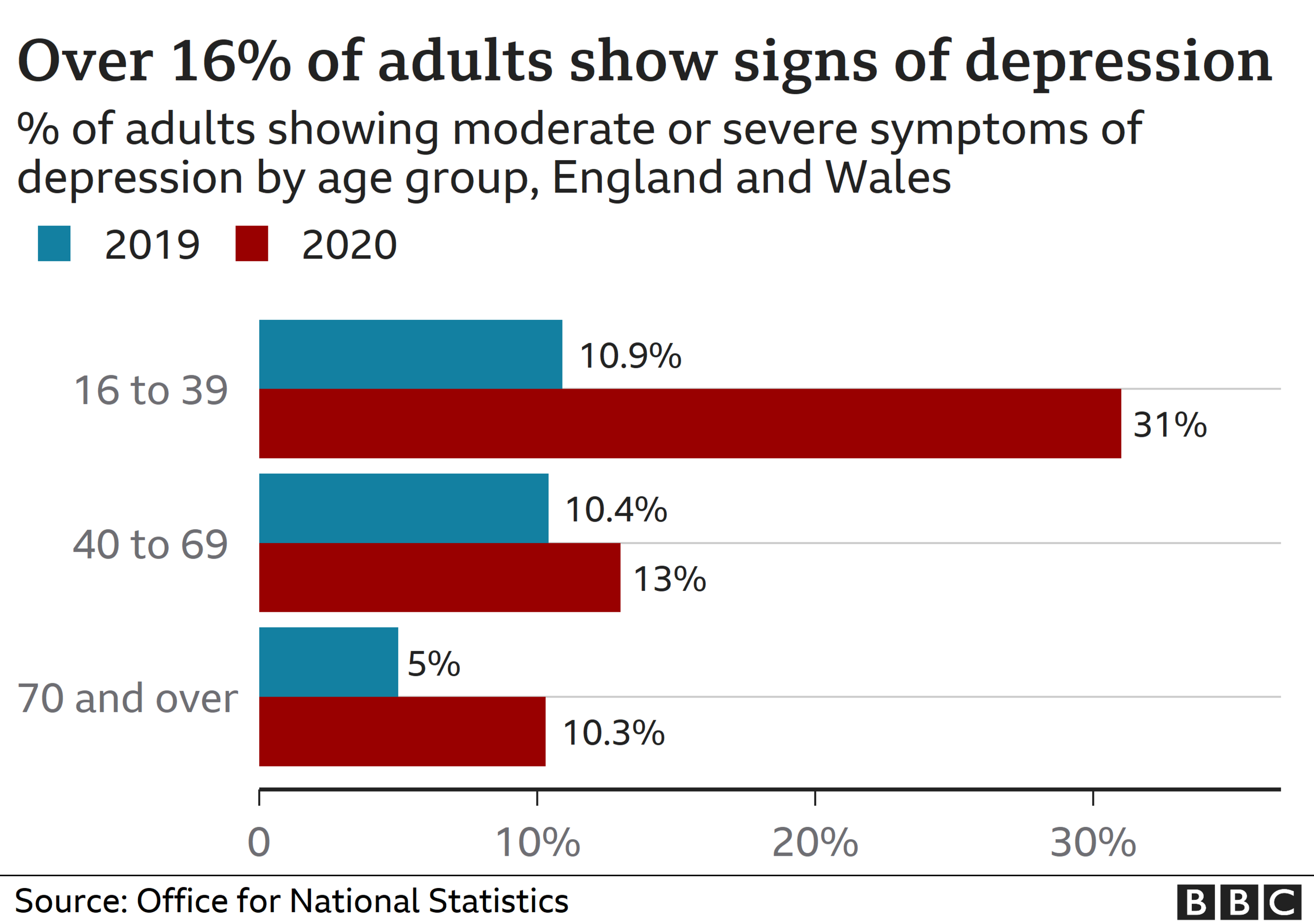
In the run-up to the first lockdown, roughly 10% of people showed moderate to severe symptoms, compared with 19% in June 2020.
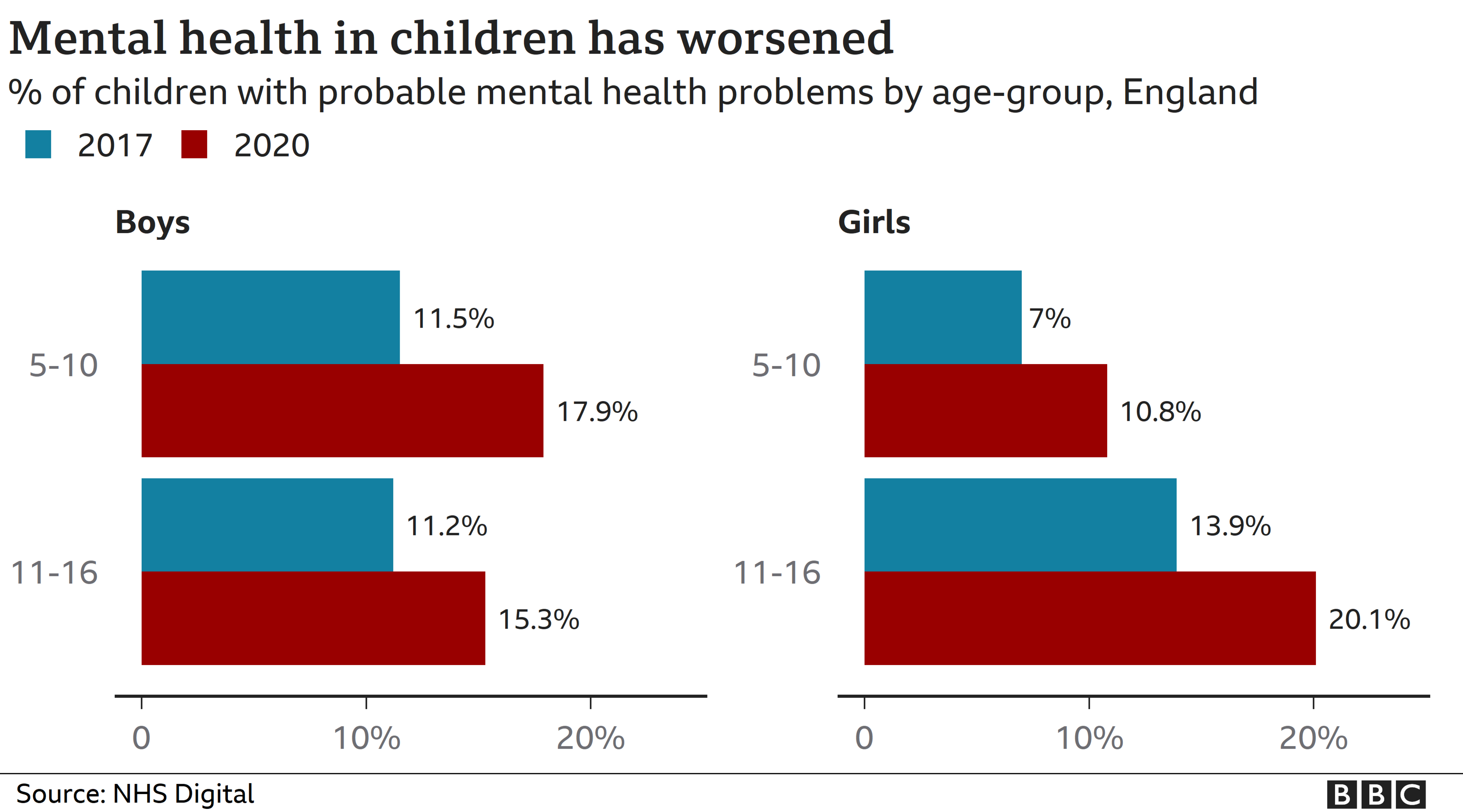
In children, 16% of 5-16 year olds have "probable" mental health disorders, external compared with 10.9% in 2017, according to NHS England.
Both of these studies are based on surveys which ask individuals questions related to mental health or depressive symptoms.
Due to the nature of mental health problems recording is difficult, but this form of survey provides the best estimates and allows for consistent comparison over time.
What issues are impacting our mental health?
Coronavirus has fuelled feelings of loneliness, anxiety and fears for the future for many people.
According to the ONS, people with depressive symptoms were more likely to feel that their finances were being impacted, as well as access to care and essential goods.
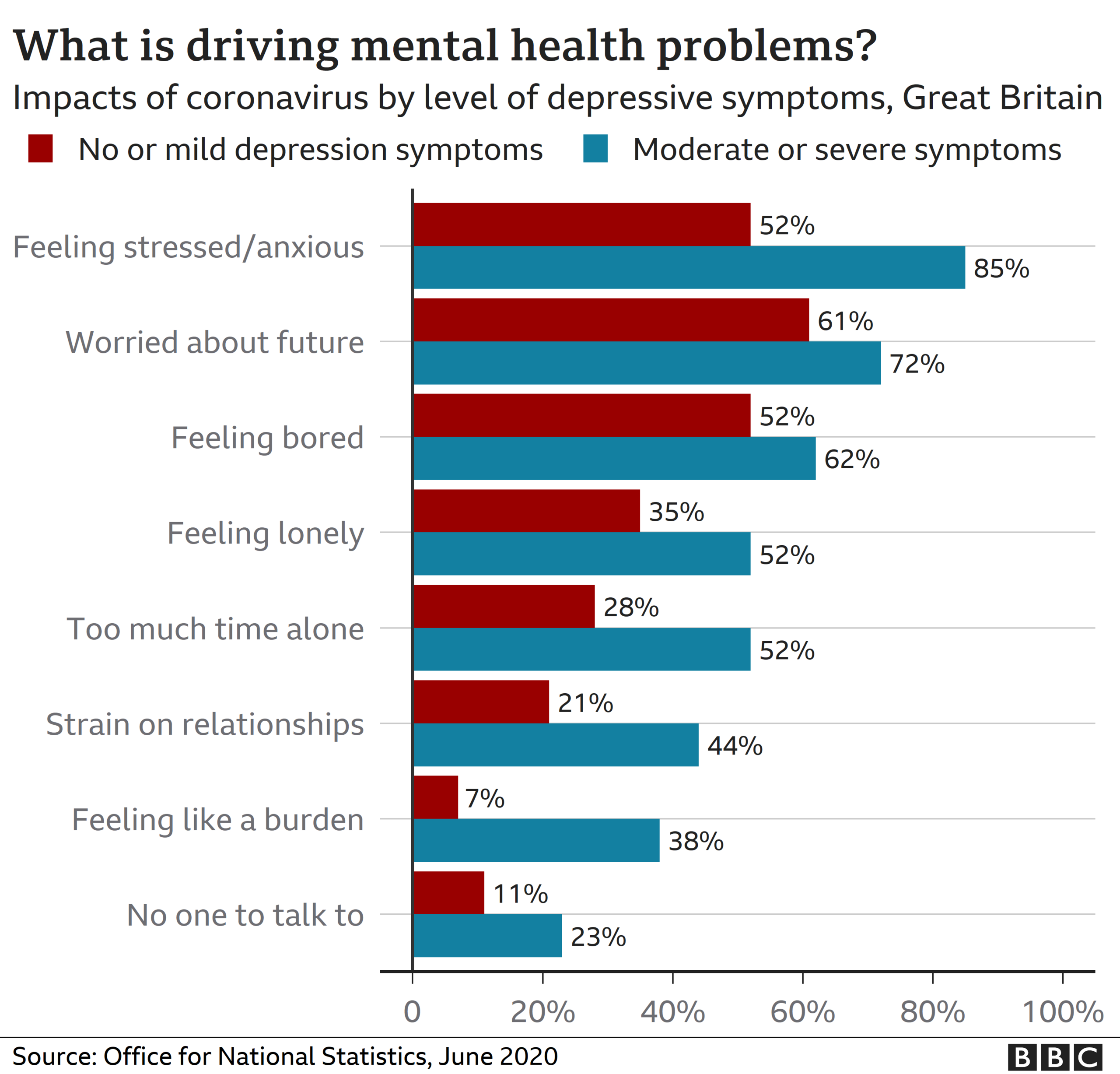
They also were more likely to feel like their personal relationships were being impacted by the virus.
Children with mental health problems were more than twice as likely to live in a household that had fallen behind with payments, according to NHS England.
They were also more likely to feel as if their lives had been made worse by lockdown.
Are people still getting help?
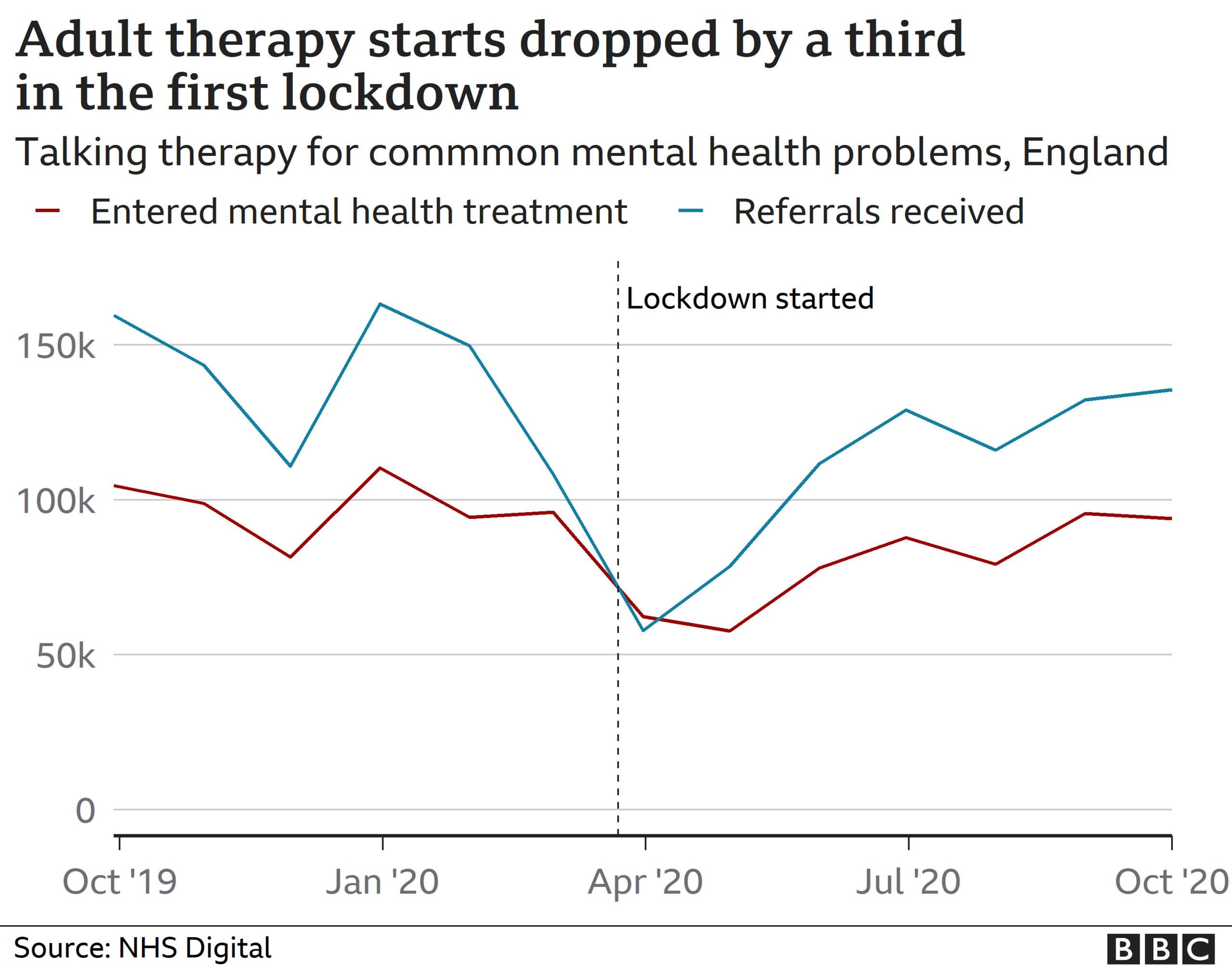
Coronavirus has had an impact on the amount of people using publicly funded mental health service.
This is part of a broader trend across the whole of the NHS.
On an average month, the NHS talking therapies service can expect to receive about 150,000 referrals for treatment of common mental health problems such as depression or anxiety.
However, this dropped as low as 60,000 in April 2020.
This slowly returned back to normal over the summer, but it is unclear how the second and third lockdowns may have impacted it.
Access to children's and teenage mental health services also saw a dip in referrals and access to treatment over the first lockdown, according to analysis by the Children's Commissioner, external.
There has been a sharp increase in referrals since then, but the increases have not been matched with similar increases in children actually accessing the services.
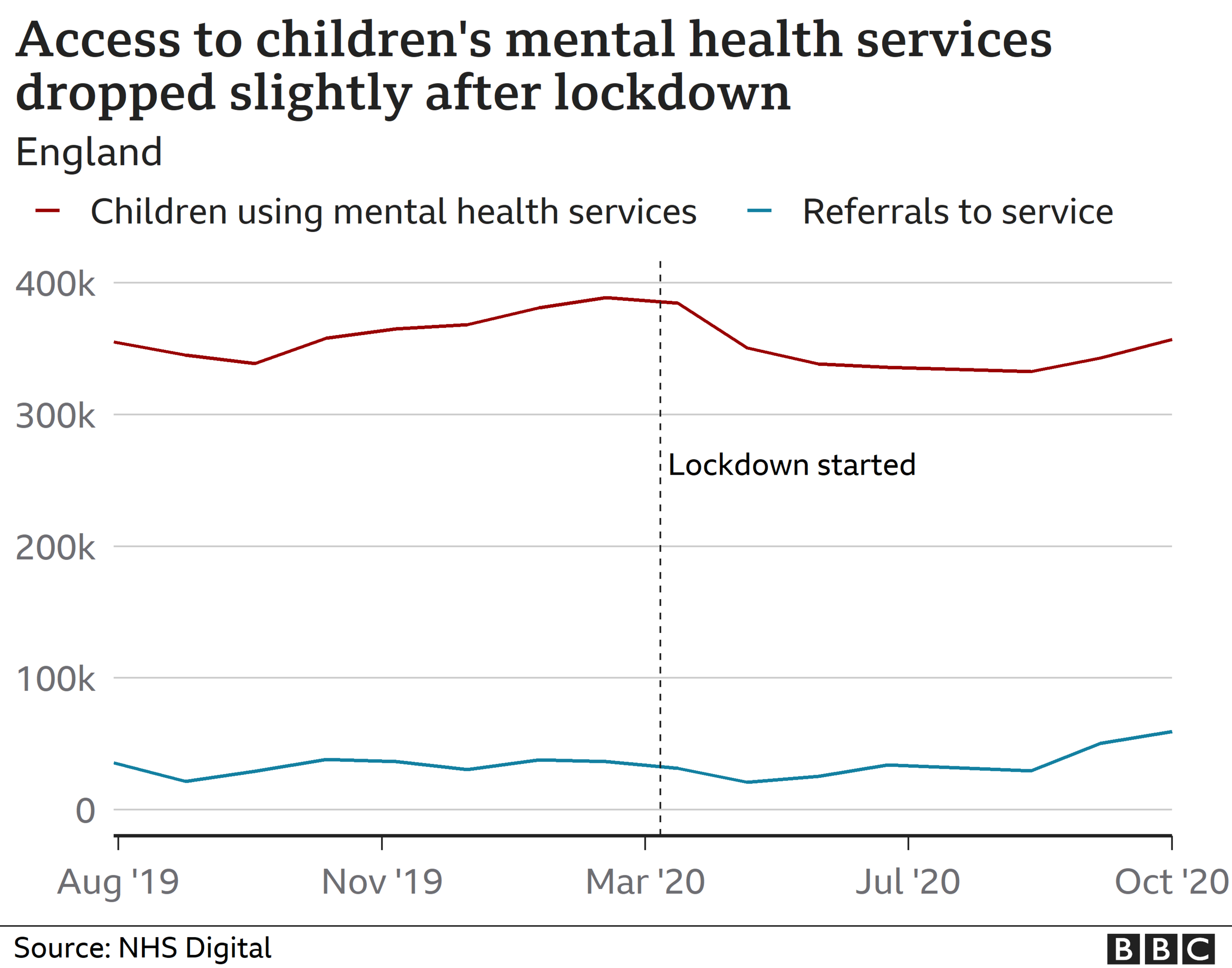
Part of these declines could be down to a big decrease in GP appointments or children not being at schools, which are often the referral point for new patients.
How quickly are people getting help?
The NHS has managed to ensure that those people who have been referred for talking therapies have been able to receive the treatment within target.
This means 95% of people are receiving treatment within 18 weeks.
Many mental health services already had the option to do therapy remotely meaning they could adapt quickly and get new patients started.
In the most recent two lockdowns, group therapy has also been considered a "reasonable excuse" to leave the home.
There isn't enough data available to check if targets for access to children's mental health are being met.

A SIMPLE GUIDE: How do I protect myself?
AVOIDING CONTACT: The rules on self-isolation and exercise
HOPE AND LOSS: Your coronavirus stories
LOOK-UP TOOL: Check cases in your area
TESTING: Can I get tested for coronavirus?

Are we seeing increases in suicide?
It's too early to say.
This is because the process for registering these kinds of deaths takes substantially more time than deaths from natural causes.
Early research from the University of Manchester, external doesn't show any major increases.
However, they say that the longer-term impacts of a future economic downturn could have an impact and that some areas could end up seeing higher figures.