Preimplantation genetic diagnosis for IVF 'is safe'
- Published
PGD testing is being used to help inform couples with a strong family history of breast cancer
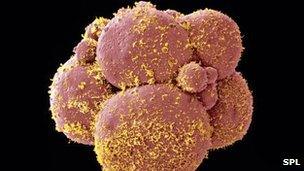
Taking an eighth of a developing embryo during IVF treatment to test for genetic diseases is "completely safe", according to the largest study of babies born following the technique.
Preimplantation genetic diagnosis (PGD) can help doctors spot diseases like cystic fibrosis before deciding whether to continue with fertility treatment.
However, there have been concerns about PGD's safety.
Experts in the UK said they were hugely reassured by the new research.
Three days after an egg has been fertilised in an IVF clinic, the developing embryo would be made up of just eight cells.
It is at this stage that doctors can delicately remove one of those cells to <link> <caption>test for more than 100 genetic diseases</caption> <url href="http://www.hfea.gov.uk/cps/hfea/gen/pgd-screening.htm" platform="highweb"/> </link> . If the embryo is given the all-clear, it can then be transferred into the woman's womb.
'Safe option'
PGD is rare, but the University Clinic in Brussels, Belgium, part of the Free University, performs about 600 PGD cycles every year.
Its data on 995 babies born through the technique between 1993 and 2008 was presented at the European Society for Human Reproduction and Embryology conference in Turkey.
It suggested the risks of low birth weight, premature birth, major malformations and the perinatal death rate was the same as for other forms of IVF.
Lead researcher Dr Sonja Desmyttere said: "Embryo biopsy does not adversely affect the health of newborn PGD children.
"It is important for parents to know that PGD is a safe option."
She advised prospective parents should "go for it," but added that research was still taking place on the impact of the test later in life.
Mr Stuart Lavery, director of IVF at Hammersmith Hospital in London, said: "This is quite an important paper.
"For many of these cases they will have been done on day three when you are removing 12.5% of the whole genetic mass of the embryo.
"So to know that is OK for the baby is hugely reassuring."
Breast cancer
Other research on PGD presented at the conference suggested that testing for hereditary breast cancer was a "good" and "feasible" option for parents.
The genes BRCA1 and BRCA2 are known to hugely increase the risk of breast cancer. Women with one of these genes have a 60% to 80% chance of developing breast cancer in their lifetimes. There is also an increased risk of ovarian cancer.
The genes can be detected by PGD, meaning embryos could be selected that do not have a heightened risk of breast cancer.
Doctors at two large fertility clinics at university hospitals in Maastricht, in the Netherlands, and Brussels, have reported 42 pregnancies after screening for BRCA genes between 2006 and 2011.
Prof William Verpoest, from the Vrije University in Brussels said: "We now believe that this technique offers an established option for those couples seeking to avoid the risk of inherited BRCA in their children."
However, he admitted this "would never be a default option" for all couples with BRCA genes, as the procedure was ethically controversial.
- Published5 July 2011