DNA test reveals 80 markers for inherited cancer risk
- Published
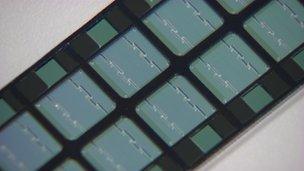
This chip was used to identify genetic markers
More than 80 genetic markers that can increase the risk of developing breast, prostate or ovarian cancer have been found in the largest study of its kind.
The DNA of 200,000 people - half of them with cancer and half without - was compared, revealing an individual's inherited risk of the diseases.
British scientists, who led the research, believe it could lead to a DNA screening test within five years.
They also hope it will boost knowledge of how the cancers develop.
The research was led by scientists at the University of Cambridge and the Institute of Cancer Research (ICR) in London and funded by Cancer Research UK (CRUK) and the Wellcome Trust.
The main findings are published in five articles in the journal Nature Genetics.
Study author Prof Doug Easton said: "We're on the verge of being able to use our knowledge of these genetic variations to develop test that could complement breast cancer screening and take us a step closer to having an effective prostate cancer screening programme."
Inherited cancer risk
The scientists looked for common genetic variations - known as single nucleotide polymorphisms (Snps) - linked to the three cancers.
Each alteration raised the risk of cancer by a small amount. However, a small minority of men with lots of the markers could see their risk of prostate cancer increase more than fourfold and for women the breast cancer risk increase threefold.
By contrast, the test can also identify those with a smaller than average risk of developing the cancers.
A woman's lifetime risk of breast cancer is one in eight, but among the 1% with lots of these newly identified genetic variations the risk rises to one in two.
The test could also help the one in 300 woman who carry a faulty gene known as BRCA1 or BRCA2. Two-thirds of them will develop breast cancer before the age of 80 and 45% who carry BRCA1 will get ovarian cancer.
At present the options to reduce their risks are limited - a double mastectomy or having their ovaries removed.
By combining the gene test for BRCA1 and BRCA2 with this extra genetic information, women who have a high number of the newly identified markers could find they have a nearly 100% risk of getting breast cancer.
In contrast, those with the protective versions of the genetic changes could see their risk drop to as low as 20%.
Dr Antonis Antoniou, CRUK senior fellow at the University of Cambridge, said: "Our research puts us on the verge of being able to give women a much more accurate picture of how likely they are to develop breast or ovarian cancer and would help to guide them about the most appropriate type and time of prevention or monitoring options for them."
Prostate
For men, the lifetime risk of developing prostate cancer is one in eight. But for 1% who carry a significant number of genetic alterations, the risk rises to one in two.
Unlike for breast cancer, there is no screening programme for the disease.
The prostate-specific antigen or PSA test, external, looks for protein markers in the blood and high levels may be an indicator or prostate cancer. But it is unreliable.
Furthermore, about two-thirds of men who get prostate cancer have a slow-growing "indolent" form of the disease that will not kill them.
Treatment options include prostate removal, radiotherapy and hormone treatment, But for every life saved through treatment for prostate cancer, it is thought that between 12 to 48 men are treated unnecessarily. Many patients opt for "watchful waiting", monitoring the cancer.
Sixteen of the 23 newly identified genetic markers are associated with aggressive forms of the disease so may help clinicians and patients decide on the best form of treatment.
Prof Ros Eeles, from the ICR, said: "These results are the single biggest leap forward in finding the genetic causes of prostate cancer.
"If further studies show such men benefit from regular screening, we could have a big impact on the number of people dying from the disease, which is still far too high."