'Golden age' of antibiotics 'set to end'
- Published
- comments
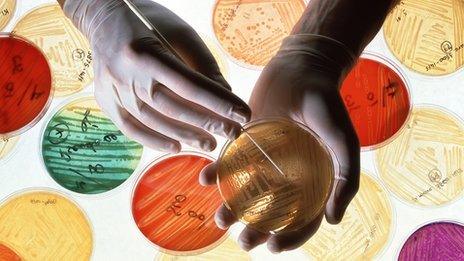
Far fewer pharmaceutical companies are working on new antibiotics than in the past
We cannot say we weren't warned. The growing threat of antibiotic resistant organisms is once again in the spotlight.
Prof Jeremy Farrar, the new head of Britain's biggest medical research charity the Wellcome Trust said it was a "truly global issue".
In his first major interview since taking up his post, external, Prof Farrar told BBC Radio 4's Today programme that the golden age of antibiotics could come to an end unless action is taken.
His comments echo those of England's Chief Medical Officer Dame Sally Davies.
Last year she described the growing resistance to antibiotics as a "ticking time bomb", and said the danger should be ranked alongside terrorism on a list of threats to the nation.
Previous chief medical officers have also warned about the threat from pathogens - bacteria, viruses and parasites.
And G8 science ministers in London discussed the danger from drug resistant infectious agents when they met in June 2013.
'Older than humanity'
But the warnings actually started many years ago.
In 1998 a House of Lords report gave this stark assessment, external: "Antibiotic resistance threatens mankind with the prospect of a return to the pre-antibiotic era."
Most of us were born into a world containing antibiotics, so it is easy to feel they are permanent fixtures in the arsenal of medicines.
In fact penicillin did not go into widespread use until the 1950s.
You can visit Sir Alexander Fleming's tiny laboratory at St Mary's hospital in London, external where he made the discovery in 1928.
But whereas antibiotics have been around for less than a century, infectious agents are older than humanity, and are continually evolving.
Two bacterial infections illustrate the problem.
Multi-drug resistant (MDR) tuberculosis is rising steadily worldwide.

The incidence of different forms of drug resistant TB is on the rise
Doctors in London have reported a sharp rise in cases of MDR TB, which can take two years to treat successfully.
That is bad enough, but there are now strains which are even worse.
Five years ago, I reported from South Africa on the growing threat of Extremely Drug Resistant (XDR) TB, external, which, as the name sounds, is virtually untreatable.
Again this illustrates that these public health threats don't spring up overnight; the warning signs emerge over a long period.
Another example is the rise in infections from enterobacteriaceae - bugs that live in the gut like E.coli and Klebsiella.
They are now the commonest cause of hospital acquired infection and some are becoming resistant to carbapenems, a powerful, last resort group of antibiotics.
There has also been an alarming increase in rates of the sexually transmitted disease gonorrhoea, which is becoming more difficult to treat.
Prof Farrar said we could have used our antibiotics better and we should have invested more in research on infectious diseases.
He said there are just four pharmaceutical companies working on antibiotics now compared to 18 companies 20 years ago.
And Prof Farrar called for industry to be given incentives to work on antibiotics and greater restrictions placed on access to these medicines.
The World Health Assembly of the WHO will discuss the issue in May.
- Published11 March 2013

- Published18 November 2013

- Published19 November 2015
- Published19 November 2015
