Statins: Are they safe?
- Published
Statins are once again in the spotlight as the NHS considers increasing the use of the drugs.
What are statins?
Statins are drugs that help to lower harmful cholesterol levels in the body by slowing down the production of cholesterol in the liver.
The drugs have been prescribed to an estimated seven million people who have been diagnosed with a 20% or more chance of developing heart disease over 10 years and to people who have had a heart attack in the past.
The NHS estimates 7,000 lives are saved by the drugs each year by cutting the risk of heart attacks and strokes.

What is being proposed?
Currently, doctors are meant to offer statin tablets to people who have a 20% chance of developing cardiovascular disease over 10 years, based on risk factors such as their age, sex, whether they smoke and what they weigh. It means about 7m people are prescribed them.
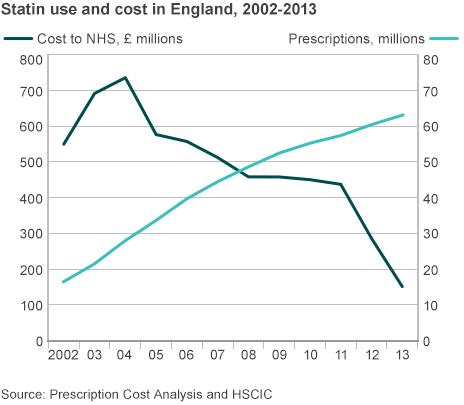
But the National Institute for Health and Care Excellence, which advises the NHS on its use of drugs, has proposed that people with as low as a 10% risk should be offered the treatment.
The draft guidance has been consulted on and a final decision will be made in the coming weeks, probably by the end of July.

So are they safe?
Every drug has side effects - even those you can buy in the supermarket, such as paracetamol or ibuprofen.
What you need to think about is: "Do the benefits outweigh the risks?" If we have a screaming headache then we all reach for painkillers despite the long list of potential side effects on the packet.
Doctors need to make a similar decision with patients when deciding whether to prescribe a lifetime of statins.

What are the risks?

Reported side effects include:
Type-2 diabetes
Muscle pain
Headache
Nausea
Insomnia
Liver inflammation
Kidney problems
Blurred vision
Nerve damage
But how common these risks are, and whether they outweigh the benefits, has become a confusing and controversial question sparking vitriolic debate within the medical profession.

What are the arguments?

Some doctors and researchers have argued the risks are too great. A survey of 500 GPs by the magazine Pulse revealed only half would personally take a statin or recommend them to a family member under new plans to give the drugs to low-risk patients.
Others say there has been an atmosphere of dangerous misinformation and compare it with the, now completely discredited, MMR-autism scare.
A review of 83,880 patients, published in the European Journal of Preventive Cardiology, external, showed there was an increased risk of type-2 diabetes, but said reports of increases in nausea, muscle ache, insomnia and fatigue were equally common in people not taking the drugs.

Isn't the British Medical Journal investigating claims about risk?

The journal published two high-profile opinion articles, which included the claim that there were side effects in 18%-20% of patients.
The authors Dr John Abramson, from Harvard Medical School, and UK cardiologist Dr Aseem Malhotra have now withdrawn their statements after those figures proved to be incorrect.
These were high-profile claims that have fuelled the debate over statins.
There is concern that the claims may have put people off taking the drugs.
The BMJ has launched an independent investigation last month to decide whether the journal should retract the rest of the two articles.

What if I already take statins?

If you have already been prescribed statins then you have a high risk of heart problems in the next decade so the benefits are likely to outweigh the risks.
However, the medicines authority NICE is drawing up plans to give the drugs to low-risk patients too who will face similar risks, but for much smaller benefits.
Decisions on taking statins should be made with a doctor.

Are there alternatives?

It is possible to lower cholesterol levels without drugs, but this requires lifestyle changes.
The NHS says, external the "most important thing to do is to cut down on saturated fat" and also advises more fruit, vegetables and fibre.
Being more active, such as running or cycling, can also help.