Legal duty over resuscitation orders
- Published
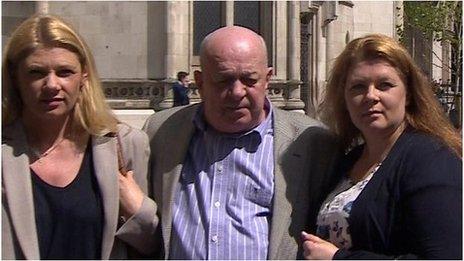
David Tracey, husband: "The fact that her death has led to greater clarity in the law gives us all some small comfort"
Doctors now have a legal duty to consult with and inform patients if they want to place a Do Not Resuscitate (DNR) order on medical notes, the Court of Appeal in England ruled.
The issue was raised by a landmark judgement that found doctors at Addenbrooke's Hospital, in Cambridge, had acted unlawfully.
Janet Tracey, who had terminal lung cancer, died there three years ago.
Her family say she and they were not consulted when a DNR notice was placed.
Guidelines for doctors already recommend that patients and families are involved in such decisions, but the court ruling now makes it a legal requirement.
In the judgement, the Master of the Rolls, Lord Dyson, said the hospital trust violated Mrs Tracey's right to respect for her private life under Article 8 of the European Convention of Human Rights.
He said: "A Do Not Attempt Cardiac Pulmonary Resuscitation decision is one which will potentially deprive the patient of life-saving treatment, there should be a presumption in favour of patient involvement.
"There need to be convincing reasons not to involve the patient."
He went on to warn that "doctors should be wary of being too ready to exclude patients from the process on the grounds that their involvement is likely to distress them".
Clarity sought
Mrs Tracey, from Ware, in Hertfordshire, was suffering from advanced lung cancer when she was taken to hospital after a serious car crash.
Her husband and daughters were distressed when a "do not resuscitate" notice was put on her hospital records.
It was cancelled after the family complained, though a second was later put in place - after talks with the family and two days before Mrs Tracey died at the age of 63.
Since her death, Janet's husband, David, has fought for a full judicial review to seek clarity over DNR notices and consent.
"It feels as though the wrong done to Janet has been recognised by the court"
Speaking after the judgement, he said: "We're all so pleased that the Court has agreed that imposing a do not resuscitate order on Janet without consulting with her was unlawful.
"It feels as though the wrong done to Janet has been recognised by the Court and the fact that her death has led to greater clarity in the law gives us all some small comfort."
Lawyers Leigh Day, on behalf of the Tracey family, said: "The judgement sends a clear message to all NHS Trusts, regulatory bodies and healthcare professionals that patients have a legal right to be informed and consulted in relation to decisions to withhold resuscitation.
"The belief such information would cause distress is no longer a sufficient reason not to inform and consult with a patient. There must now be convincing reasons to displace this right."
The ruling does not give patients the right to have CPR, but it does mean they should be consulted.
Dr Keith McNeil, the head of Cambridge University Hospitals NHS Foundation Trust in charge of Addenbrooke's, said: "Today's ruling hinges on a specific point of law. There was no criticism of our clinical care.
"It is a fact of life that every day people die in hospitals. From my own experience as a specialist hospital doctor, the most important thing is that these patients are treated with the utmost respect and dignity."
A Department of Health spokesperson said: "It is important that doctors follow the very best practice so standards of care in this in area can be improved. We will continue to work with professional bodies to make sure guidance is understood by health professionals."
The General Medical Council said it would check whether it needed to update its current advice.

Do Not Resuscitate - By Daniel K. Sokol, barrister and medical ethicist
The decision by the Court of Appeal that the placing of a DNR order on Janet Tracey's medical notes without her knowledge was unlawful is a warning shot for all hospitals in England.
Doctors will need to justify DNR decisions and should make sure they keep a contemporaneous note about the discussions they have with the patients and families involved.
The Court held that if a patient has capacity there should be a presumption that they should be involved in the DNR decision.
There must be 'convincing' reasons not to involve the patient - a clinician's belief that cardio-pulmonary resuscitation will fail is not enough. Neither is the fact that the patient may find the topic distressing.
However, if the clinician believes that involving the patient in the process will cause the patient physical or psychological harm this could count as a convincing reason.
This is the most problematic part of the judgment. The boundary between distress and psychological harm is unclear. Clinicians may attempt to justify their decision not to involve patients by claiming that disclosure would probably lead to psychological harm.

- Published19 December 2012

- Published8 May 2014
