The NHS budget: Five things we've learned
- Published
- comments
The NHS budget is under the microscope like never before. The coalition may have protected it, but that has not stopped problems mounting.
Earlier this week a host of medical organisations wrote a letter to The Times, external warning the NHS was "creaking at the seams".
The Nuffield Trust think-tank has now published what is probably the most in-depth look at finances in recent times.
The headline warning is that health care leaders fear the NHS may stop being free at the point of use within a decade. But the report reveals much more than that.

The piggy bank is being raided

Much of the focus is on the deficits being run up by hospitals. That is understandable - they are the public face of the health service.
But the accounts of the bodies that control the overall £100bn-plus health budget - NHS England and the GP-led clinical commissioning group - are more revealing.
They finished 2013-14 just over £250m in surplus, but that was only because they took nearly £400m from their reserves. There is now less than £800m stashed away. The room for manoeuvre is getting tight.

Hospitals have Stafford on their mind

The guidelines say there must be enough nurses to give patients the assistance they need
Following the public inquiry into the Stafford Hospital scandal, a popular saying has developed among hospital bosses: it is better to be hung for finances than the quality of care.
The Nuffield Trust reports shows they have been as good as their word.
Last year saw a rise in the number of staff employed by hospitals by 18,000 - a 1.6% increase in total. Foundation trusts - the top performing organisations - spent an extra £1.2bn alone - £660m more than planned.

The NHS is off the pace

Next year will see the NHS come to the end of a five-year £20bn productivity drive. The challenge was for the health service to make efficiency savings of about 4% a year.
This is something it had never achieved before, but the health service rose to the challenge. Initially at least.
In the first couple of years it was on target - largely because of wage freezes - but 2013-14 could be the year it started to unravel.
Managers reported productivity gains of £1.7bn - about half of what they should have.

The revolution hasn't happened
The answer to the rise in long-term conditions, such as diabetes and heart disease, which account for 70% of the NHS budget, is to shift care out of hospital and into the community.
The theory is that this is more efficient and more likely to help people keep well and independent.
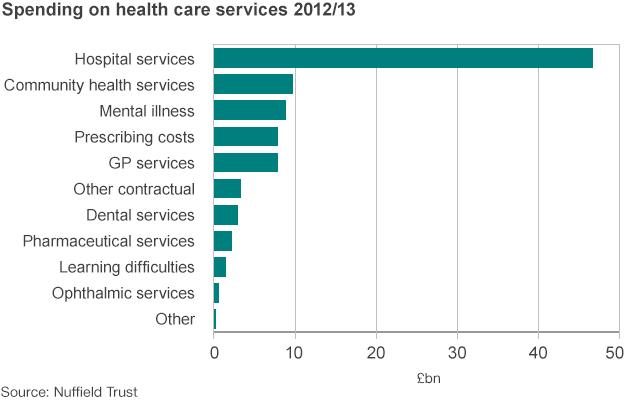
But there appears to be little progress. Both emergency admissions and outpatient appointments are up and hospital spending still accounts for over half the NHS budget.

There is a great divide

It is clear from wading through the NHS accounts over the past few years that when it comes to hospitals there are the haves and the have nots.
The largest trusts - often the big city hospitals - remain in the healthiest position financially.
Take 2012-13, for example, the 27 biggest trusts posted a surplus of nearly £200m, but that was cancelled out by the smaller and medium-sized trusts.
It raises question marks over the future of a whole network of district general hospitals that seem to be struggling to attract enough patients to remain viable.