Sepsis: Antibiotics 'not working'
- Published
- comments
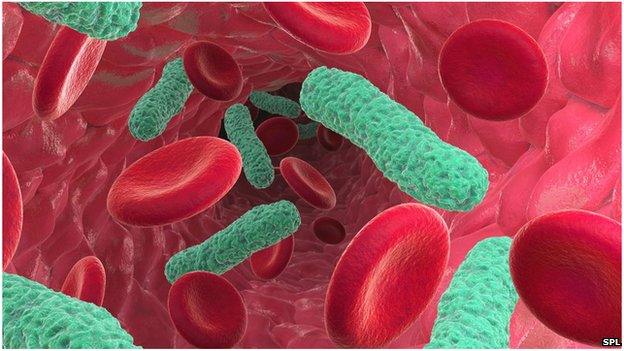
Sepsis is a potentially fatal condition caused by the body's immune system overreacting to infection
Patients are dying from sepsis because of a lack of effective antibiotics, an expert is warning.
Mark Bellamy, president of the Intensive Care Society, told the BBC the problem of resistance would get worse unless new and effective antibiotics were developed.
Sepsis is triggered by infections and causes around 37,000 deaths a year in the UK.
NHS England says hospitals should work together to tackle the problem.
Prof Mark Bellamy: "Without new and effective antibiotics the problem will gradually escalate"
Sepsis usually develops from blood poisoning and involves a dramatic reaction by the body's immune system.
If not treated quickly it can lead to organ failure or death.
Early symptoms can include a high temperature and a fast heartbeat.
Deadly
The Intensive Care Society recently launched a campaign to raise awareness of sepsis to avoid what it says are thousands of preventable deaths.
There are 37,000 deaths a year in the UK because of sepsis, compared with just more than 35,000 from lung cancer and 16,000 from bowel cancer.
The society, along with the UK Sepsis Trust, argues that there is inadequate recording of sepsis cases by hospitals and insufficient knowledge of the steps required to recognise and treat it early.

Case study
Julie Bignone nearly died because of sepsis and spent seven weeks in hospital - some of them in a critical condition.
Feeling feverish, she assumed she had a bad dose of flu. After a weekend in bed, she went to her GP and was told to come back if her condition worsened and antibiotics would be prescribed.
But later that day, with her family growing more anxious she was taken to hospital by ambulance.
Julie was found to have pneumonia in both lungs and sepsis and doctors feared she might not survive.
She only pulled through after several weeks in intensive care and heavy doses of antibiotics.
She feels now that she should have acted on her instinct early on that she was suffering from something a lot worse than flu.
Julie says: "There's a lot of scope for getting it wrong with sepsis because the symptoms are not specific enough - we need to get a system where doctors listen to patients more and allow them to have more of an opinion".

Failing antibiotics
Prof Bellamy, who is based at the Leeds Institute of Biomedical and Clinical Sciences, said: "For the first time this year I have had a couple patients for whom we had no effective antibiotic treatment, it's rare - but two years ago it would still have been regarded as a theoretical problem."
He says it is crucial to raise the profile of sepsis, and to ensure it is tackled early to give the patient the best chance of survival.
The diminishing impact of antibiotics, in his view, underlines the urgency of the task.
He said there was a "spectre emerging of moving into a post-antibiotic era".
NHS England has acknowledged the scale of the problem.
Bruce Warner, its deputy director of patient safety, said: "We know there are many preventable deaths due to sepsis each year and our top priority has to be saving those lives we can save and having as big an impact as we can."
NHS England wants to encourage greater co-ordination within hospitals to ensure sepsis is diagnosed and treated quickly.
It cited Nottingham University Hospitals Trust, which has been praised for use of laptops by staff to record patient data and symptoms and ensure they are analysed quickly by clinicians.
- Published12 September 2013
- Published17 October 2013

- Published1 February 2013
