How much is a year of life worth?
- Published
- comments

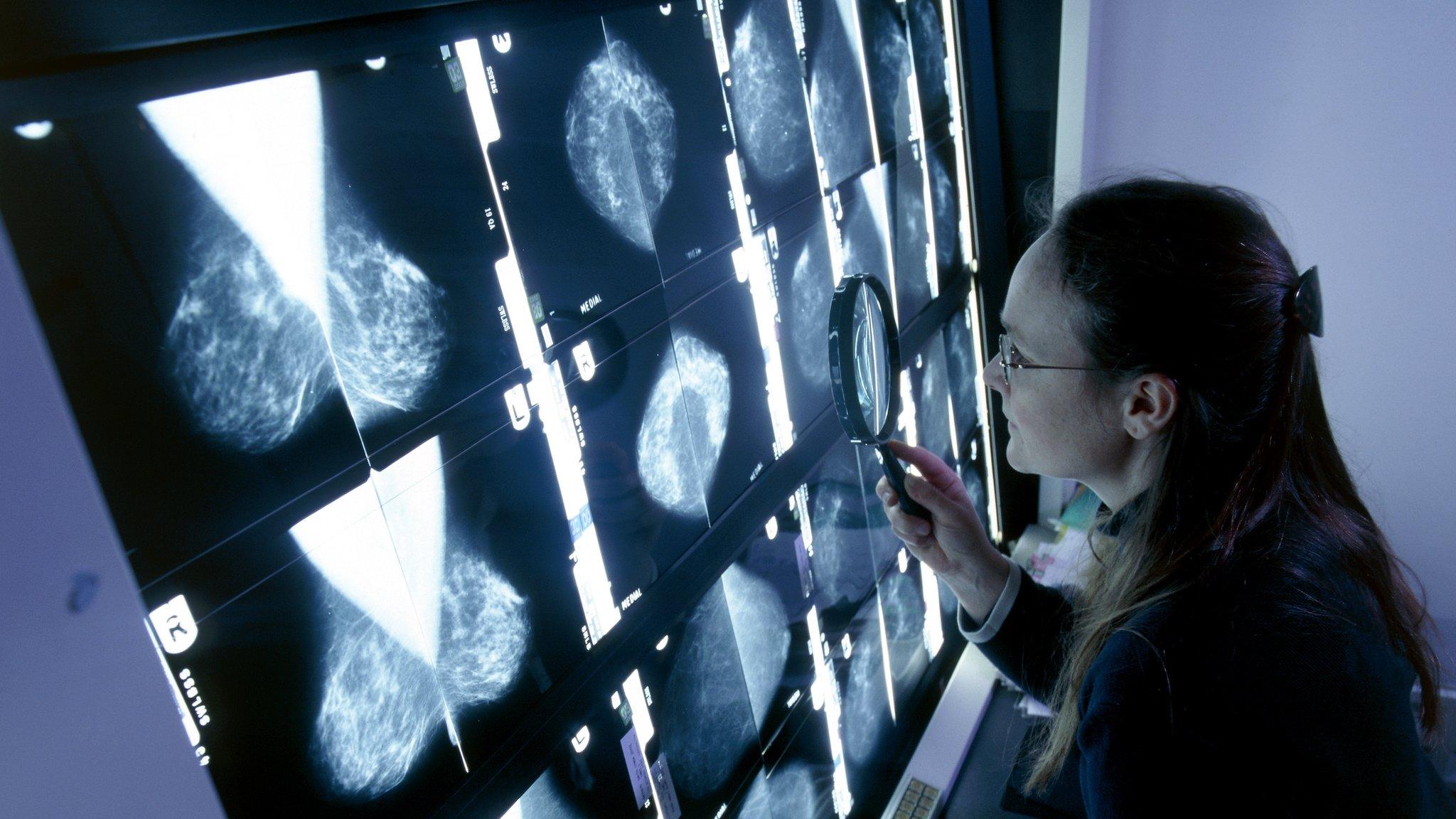
Drugs for cancer patients are often very expensive
Thinking about the cost-benefit decisions on the affordability of drugs made by the National Institute for Health and Care Excellence (NICE) involves a grim question: how much is a year of life worth? How much should you, the taxpayer, be willing to pay to keep someone alive?
Earlier this week, Newsnight ran an exclusive story about new proposals that would see officials in NHS England threatening to stop buying some cancer drugs if the companies that make them do not agree to cut their prices.
Officials think that the Cancer Drugs Fund, a pot of cash to pay for drugs deemed too expensive for the normal NHS England processes, leads to them overpaying for some chemicals.
One curiosity worth exploring a bit more in this saga is how one thinks about those kinds of cost-benefit decisions, which in the UK are mostly made by NICE.
NICE uses a unit of measurement called the "Qaly" - the "quality-adjusted life year". It gauges drug effectiveness in terms of how much it would cost to give you a year of healthy life.
So a drug that cost £50,000 and gave patients an extra six months of life in good health would cost £100,000 for a full Qaly. If the same drug at the same price was much better, and led to two years of life in good health, it would cost about £25,000 per Qaly.
Patients are also deemed to "gain" Qalys for periods of better health. That means that an intervention that does not prolong life, but does improve it, could be justified for funding. That's what the "quality-adjusted" bit in "Qaly" means.
NICE aims to spend less than £20,000 to £30,000 per Qaly. That is not a hard limit; it will go almost twice as high for end-of-life drugs. NICE accepts that, at the very end, a small amount of extra time can seem to be worth a lot more to patients and families.
Cancer Drugs Fund
But NICE does impose limits. And cancer drugs, in particular, often cost much more than that and so get refused by NICE for being too expensive.
At the moment, cancer patients in England are shielded from that problem; the Cancer Drugs Fund pays for drugs for them, regardless of cost. So far, 55,000 patients have been bought drugs not offered by the normal channels.
But patients outside England have not been included. And there are two big reasons why cancer drugs are increasingly hitting the NICE cost barrier.

High-tech drugs may be more effective, but they only work for small numbers of people
First, the amount that NICE is willing to pay per Qaly has, in effect, been falling every year since 1999; it has not adjusted with inflation. The NHS is willing to pay less in real terms for life than it was in Tony Blair's first term.
The Qaly price is also not stunningly high. For example, there is a discrepancy between the £20,000 to £30,000 limit used ordinarily by NICE and the £80,000 per Qaly that the Home Office is willing to pay.
Cost-effective?
There are strong reasons not to raise the Qaly limit; for example, some economists think that the price is actually too high.
So NICE is approving things that are less cost-effective than lots of boilerplate treatments.
As a result, hospitals have, in some cases, had to cut more cost-effective treatments to fund new but expensive and less efficient ones approved by NICE. Raising the Qaly threshold would encourage more of that.
It would also fuel drug price inflation (and the NHS, aided by a frozen Qaly, is quietly rather good at squeezing the pharma industry for boilerplate drugs).
But the simple process of inflation in the outside world means that the conveyor belt of drugs developed recently are more likely to bust cost limits. It just costs more to make stuff than it did.
Not cheap
Second, costs for cancer drugs are high because of the changing nature of pharma: high-tech drugs are more effective, but work for small numbers of patients.
If you leaf through NICE documents, drug regimens for cancer that might help fewer than 2,000 patients a year are common. Yet they are not cheap to make. So the result is a very high cost per patient.
NICE is working on new measures for gauging effectiveness, and how the NHS responds to its rules. That might change which drugs we think are good value for money.
But some things are unavoidable; more higher cost treatments are coming through. And if we want to spend money on them, we either have to spend more overall or find other ways to cut the health budget.
- Published27 August 2014
- Published7 August 2014
- Published8 August 2014