The NHS plan: Five things we've learned
- Published

The unveiling of the NHS Forward View has been anticipated for some time.
Six key national health bodies have put their name to it, but it is hard not to see it as the vision of the new leader of the health service in England, Simon Stevens.
He started in post in April but has kept a low profile so far.
The document is brief - it runs to fewer than 40 pages - but it certainly packs a punch, setting out a template for how the service in England needs to change over the next five years.

Money matters

NHS officials normally steer clear of speaking about the size of the budget. It is seen as a matter for politicians.
Not this time. At the press briefing, Mr Stevens and David Bennett, the chief executive of regulator Monitor, clearly set out what was needed.
The £30bn shortfall figure for 2020 was already well established.
And the pair were clear that the NHS could become more efficient and meet over two-thirds of this.
But they said the rest - £8bn by 2020 - needed to come from government. It amounts to an extra 1.5% a year on top of inflation.
It will make it hard for any political party not to agree to funding increases in the run-up to the next election.

Small hospitals have a future
Much has been made of the demise of smaller hospitals. For years the great and the good of the health service have been saying some will need to close.
But this document is clear, that is not necessarily the case.
It talks about small hospitals working together to share back-office and management functions, such as HR and admin.
It also floats the idea of big hospitals opening franchises at these smaller sites, much as you see Costa coffee shops or McDonald's restaurants in airports and leisure centres.
Moorfields Eye Hospital has already done this. It has 28 clinics across London.
Some of the big cancer hospitals are exploring doing the same.

But there is no desire for any more

One of the biggest factors for the £30bn funding gap is the rising number of people being admitted to hospital.
The Nuffield Trust has estimated a quarter of the shortfall is linked to the rising rate of admissions. Over the past six years, hospital admissions in England have risen by 16% to over 14 million a year.
If this continues, by 2022 it is estimated another 17,000 hospital beds will be needed - the equivalent of 22 hospitals.
But Mr Stevens was clear this was not a wise use of money. Instead, much of what he has put forward is designed to stem this rise by improving how patients are looked after in the community.

The barriers are being ripped down
Ever since the NHS was created in 1948, it has divided into two broad areas - GP care and hospital care.
With the possible exception of mental health, virtually everything else falls into one camp or the other.
But the report is clear this must change. GPs practices, it says, should be open to employing hospital doctors and nurses so they can expand into new areas.
Meanwhile, hospitals could open their own GP clinics if they wanted, the report adds.
It is probably no coincidence that the plans mirror - to some extent - the situation in the US, where Mr Stevens used to work. There, the lines are much more blurred between hospital and community care.

The time for talking is over
This is not the first time the NHS has been told to move care out of hospitals. It has been the mantra for the past decade or more.
So what makes this push different? Mr Stevens was clear. He said the health service simply had "no choice".
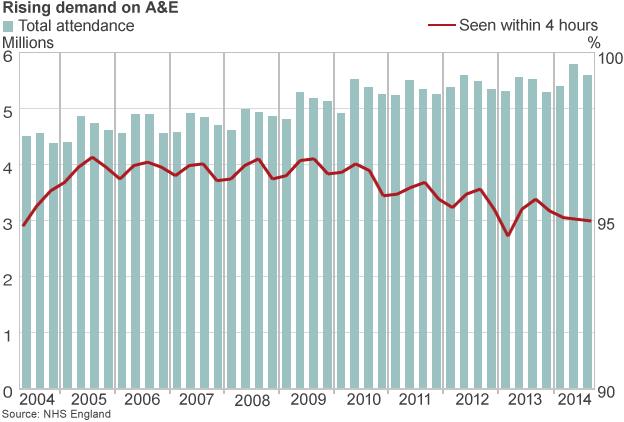
The tight funding situation coupled with the rising pressure on services (the graph above is an illustration of this) means the NHS has no wriggle room.
Mr Stevens went on to say he would be keeping up the pressure on politicians in the lead up to the election and moving "heaven and Earth" to make sure the NHS on the ground responds.