'I don't fear death'
- Published
- comments

Adrian and Christine Small at Thames Hospice in Windsor
"I don't fear death" says Adrian Small.
The 68 year old has terminal pancreatic cancer.
But pain does worry him. His cancer causes excruciating discomfort which can be controlled only through massive doses of morphine-like drugs and other medication.
"I get a really bad thumping pain" he says, "but within half and hour of taking the tablets I feel fine."
Mr Small is on his sixth in-patient stay at Thames Hospice in Windsor, Berkshire.
On several occasions he has been close to death.
Superb
Married to Christine for 43 years, the couple say the palliative care at the hospice is superb.
Mrs Small says: "The staff here know Adrian needs very big doses of painkillers - they are used to dealing with it - but when we are in a general hospital the doctors are frightened by the numbers and they won't give him what's needed."
The couple have never considered an assisted death since Adrian's diagnosis.
Mrs Small says: "It's not been about dying it's been about living for two years - everybody deserves the dignity you get here".
But the hospice - which has 17 beds in Windsor cannot help all those who could benefit.
It's Chief Executive, Debbie Raven says: "Every day we have up to 13 people waiting for one our our in-patient beds, so inevitably we have to turn some patients away; we'd like everyone to have access to high quality palliative care no matter where they are."
The hospice does not take a stance on the issue of assisted dying, nor does it judge those who are for or against a change in the law.
Fear
The medical director, Dr Cecily Wright says they do sometimes get asked to end a patient's life: "We do occasionally - that request is often coming from a place of great stress and fear.
"It's very seldom just about pain and that's why we use our holistic approach to bit by bit make life easier and better."

Lord Falconer's Bill ran out of time
I spoke to Adrian and Christine on the eve of a debate on assisted dying in the House of Commons.
Labour MP Rob Marris is proposing a bill, external which would allow doctors in England and Wales to prescribe a lethal dose to terminally ill patients judged to have six months or less to live.
A judge would review all decisions and rule whether a person was choosing an assisted death free from coercion.
Currently, assisted suicide is illegal under the Suicide Act 1961, external and is punishable by up to 14 years in prison.
The private member's bill is almost identical to one introduced in the House of Lords last year by the former Lord Chancellor Lord Falconer, and which ran out of parliamentary time.
Free vote
It's the first time since 1997 that a bill of this kind has been brought forward in the Commons.
MPs will be given a free vote, but even if the bill gets through its second reading, it is very unlikely to succeed as it lacks government backing.
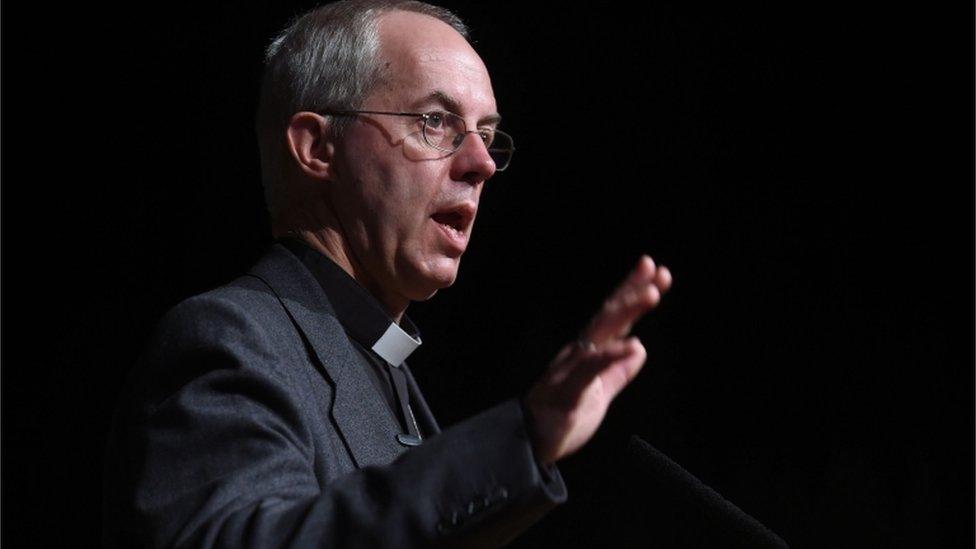
Justin Welby has expressed concerns
Campaigners in favour of changing the law point out that about one Briton a fortnight travels to Switzerland to end their life with the help of the suicide organisation Dignitas.
Those opposed argue it would send a message that, if you are terminally ill, taking your own life is something it is appropriate to consider.
The campaign group "Living and Dying Well" said it would expose vulnerable people to pressure to take their own lives.
The Archbishop of Canterbury described assisted dying as one of the "biggest dilemmas of our time", but dismissed suggestions that current laws are not working.
Justin Welby said the evidence around the world is there is a "slippery slope" and once you accept the role of medicine is deliberately to kill people, there would be pressure to go further.
California has just approved similar legislation, external, modelled on a law in Oregon which allows terminally ill patients to obtain a lethal dose to end their lives.
- Published9 June 2015

- Published26 May 2015