Why the NHS needs better-behaved patients
- Published
- comments

What does the NHS want for Christmas? More money? Yes. More staff? Yes again. But, whisper it quietly, better behaved patients wouldn't go amiss either.
In fact, in their more candid moments, it's not unusual to find doctors and nurses having a little moan about the people they care for.
Why? Well when the health service is under so much pressure and scrutiny as it struggles with deficits and to hit its targets there seems to be a creeping exasperation with the way some patients use - or perhaps that should be abuse - the system.
There are numerous examples of this. Patients not turning up for appointments is a big bugbear.
Figures show that about 12 million GP appointments are missed each year - about 4% of the total. It costs the NHS over £160m a year. To put that in context, it's enough to pay for another 7,600 nurses.
A further 5.5m hospital appointments are also missed - about one in 10 - at an average cost of over £100 a go. The waste is clear for all to see.
The NHS has been doing its bit to reduce these costs in recent years by increasing the use of email and text reminders, but the onus is quite rightly on patients.
Drug treatment
The same could be said for completing courses of drugs. The dose and duration of a prescription is determined by evidence of what works best in order to successfully treat patients. Stopping early, even when the symptoms may have gone, can lead to the illness recurring and, in the case of viruses or bacteria, drug resistance developing.
But large numbers of patients are failing to finish their treatment. Research by Aston Pharmacy School, external two years ago found as many as one in three patients were not adhering to their prescriptions.

How patients use the emergency end of the system is also a source for concern.
Stories of pointless 999 calls to ambulance services crop up from time to time. In recent years we have heard about one woman ringing to ask for her washing to be brought in because it was icy and a caller who wanted paramedics to see if they could resuscitate a dead pigeon.
But the problem runs much deeper than a handful of wacky calls. Estimates suggest that between 15% and 40% of visits to A&E are not needed.
Drinking is an obvious source. Only this week figures from the Nuffield Trust think tank showed hospital visits for alcohol poisoning have doubled in six years, with the highest rate among females aged 15 to 19.
Some are serious cases of poisoning and lead to people being admitted for vital treatment. But many are dealt with there and then by hard-pressed staff in the A&E department who are struggling to keep up with the record number of patients who are turning up.
Overall, alcohol misuse costs the NHS about £3.5bn a year - or £120 for every taxpayer.
But drinking is just one element of how we live our lives is having an impact on the NHS.
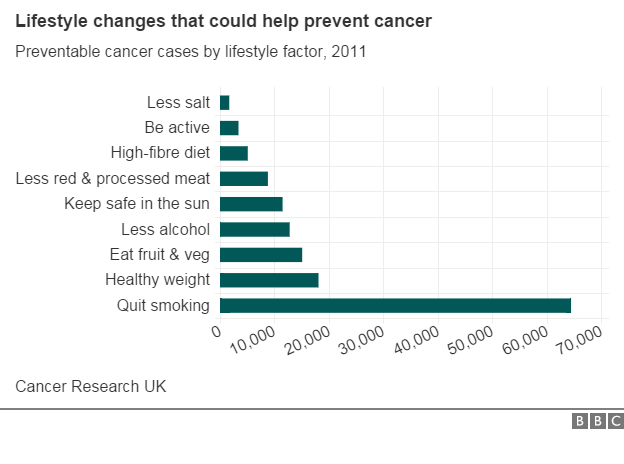
Physical inactivity, smoking and diet are all linked to a range of diseases from cancer to diabetes and liver problems. About four in 10 cancer cases alone are linked to lifestyle factors.
All this matters. While the NHS is getting more money - an extra £8.4bn in real terms this Parliament in England - that is twinned to increasing efficiency and preventing ill-health.
Of course, there are things the NHS can and should do itself. But part of the answer also lies with us, the patients.