Hospital bed-blocking 'costs' NHS England £900m a year
- Published

Delays in discharging patients out of hospital after treatment could be costing the NHS in England £900m a year, an independent review has said.
Labour peer Lord Carter's report found nearly one in 10 beds was taken by someone medically fit to be released.
It said it was a "major problem" causing operations to be cancelled and resulting in the NHS paying private hospitals to see patients.
Union Unison said cuts to social care were a major cause of "bed-blocking".
Lord Carter identified the issue in a wider look at how £5bn could be saved by 2020.
His proposals called for better procurement and staff management, and savings to the drugs bill.
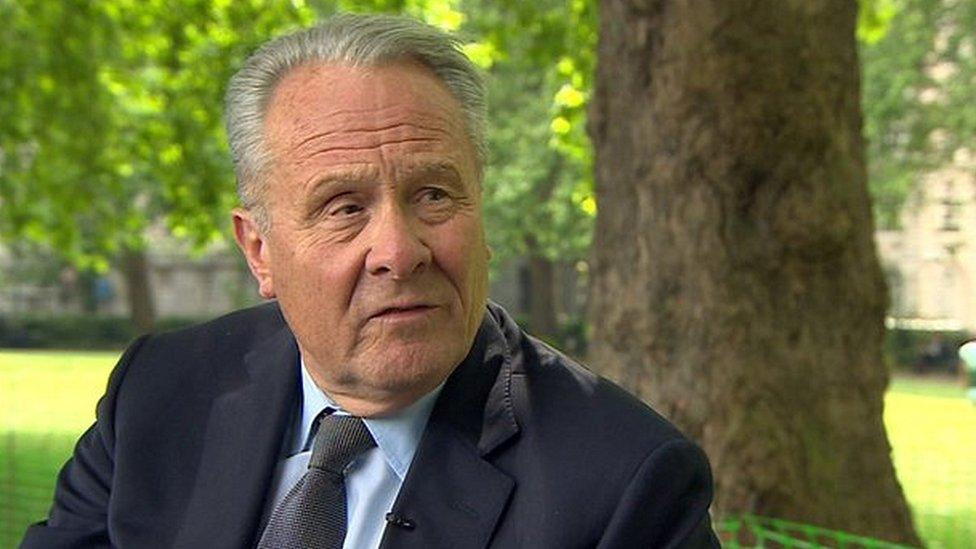
Lord Carter says the NHS in England could save £5bn a year with improved staff organisation and better buying practices
But delayed discharges are likely to be prove a more intractable problem as it is largely not down to the actions of hospitals.
Vulnerable and frail patients cannot be released if there is not the support in the community from home care workers or district nursing staff or a place in a care home.
While official statistics suggest about 5,500 patients a day are affected, the report said information provided by trusts estimates as many as 8,500 beds in acute trusts were being blocked.
It said if you take into account how much staffing and running a bed costs this works out at £900m a year.
But the true cost could be even higher. The report highlighted the growing trend to pay private hospitals to do NHS work, such as knee and hip operations, as a consequence of this.
Last year the NHS spent £11bn in the private sector - a rise of 11% on the previous year. Lord Carter said delayed discharges was likely to be a "contributory factor" in this.
Delayed discharges have also been blamed as one of the causes of growing waiting times in A&E as doctors struggle to find beds for patients who need to be admitted.
Meanwhile, Lord Carter said hospitals across England must end "stark" differences in spending and productivity, Lord Carter added.
He found the average cost of an inpatient treatment is £3,500 but said there was 20% variation between the most expensive trusts and the least expensive.
'Major problem'
Lord Carter said: "My experience of the NHS and hospitals internationally is that high-quality patient care and sound financial management go hand in hand."

Analysis: Savings target is just a start
Hospitals consume £55bn of health spending - about half the annual budget. So a £5bn efficiency target is very ambitious.
But as a sign of the mountain the health service has to climb in the coming years, consider this: it doesn't even go a quarter of the way to achieving the overall savings the health service is aiming for.
In return for the extra £8bn it is getting this Parliament, the NHS has pledged to save £22bn.
It means the rest will have to come from people improving their lifestyles (and so preventing ill-health), moving care out of hospitals and into the community (which is cheaper) and keeping tight control on salaries. It promises to be a tough few years.

Lord Carter, who published an interim report in the summer, identified the following savings:
£2bn through better management of staff with sickness and absence rates varying between 3.1% and 5% of staff
£1bn on procurement - the prices paid by different hospitals for hip replacements vary from £788 to £1,590 for example
£1bn from the better management of estates, such as lighting, heating and utilising floor space, with one trust using just 12% for non-clinical purposes, while another used over two-thirds
£1bn through the drugs bill by making greater use of cheaper generic medicines and cutting back on wasted stock
Each hospital has been set its own individual savings targets. These are not being released publicly although the progress trusts make will be monitored.
Ministers said they expected the savings to be made.
Christina McAnea, head of health for Unison, which represents many NHS workers including nurses, paramedics and administrative staff, said the report contained many good ideas.
However, she said the report failed to address the lack of social care in the community that was the "main reason why people can't be discharged".
"On average social care has been cut by around 25% and that has an almost immediate knock on effect in the NHS, because you can't discharge patients unless you've got the infrastructure back in the community to support them," she said.
"And that's where we've seen massive cuts, so it's about care workers, some community nursing, it's about health visitors."
Health Secretary Jeremy Hunt said: "This ground-breaking review will help hospitals care for patients, making sure every penny possible is spent on front line patient care and bureaucracy is slashed so doctors and nurses can concentrate on caring."
Shadow health secretary Heidi Alexander said: "This report is absolutely right to highlight the huge financial pressures that delayed discharges are placing on the NHS. However, ministers cannot shy away from the fact that this is a crisis in care that has happened on their watch."
- Published21 October 2015

- Published11 June 2015

- Published31 May 2015

- Published22 May 2015
