Newborns at risk from deadly Group B Strep bacteria
- Published

Aimee Heath who was left with disabilities as a result of being born with the condition
"When the midwife came to the house, Aimee went floppy and unresponsive and the midwife called for an ambulance straight away.
"It all happened very quickly. They told me that she had a 5% chance of surviving."
Charlotte Heath, 28 and from Cheslyn Hay near Walsall, fights back the tears as she recalls the moment she was warned her five-day-old daughter may die.
Little Aimee had been infected with early onset Group B Streptococcus (or GBS) which, while harmless in most cases, can lead to a range of serious illnesses, including septicaemia, pneumonia and meningitis within the first week of a baby's life.
The bacteria - carried by an estimated one-in-four pregnant women - is passed from mother to baby.
In the majority of cases, babies can be protected if the mother is given intravenous antibiotics during labour.
But Charlotte did not know she was a carrier.
Aimee was left with a series of disabilities after contracting Group B Strep infection
Despite the bleak outlook, Aimee survived but has been left with quadriplegic spastic cerebral palsy which means that she cannot sit unaided, walk or talk.
Charlotte said: "I know people will probably look at me and say, 'you know, she's got all these problems, you're fantastic, I don't know how you cope', but you do, you just get on with it because you know it could've been different.
"We feel lucky to have her."
Public Health England, which collates data for England, Wales and Northern Ireland told 5 live Investigates that the number of babies being made ill by the infection has increased by 12% between 2011 and 2015.
According to the British Paediatric Surveillance Unit, 518 newborn babies in the UK and Ireland were made ill as a result of the bacteria, 27 died and dozens more like Aimee were left with disabilities in the year to April 2015.
He died 20 minutes later
Craig White and Lynsey Dalvarez's son Frankie did not survive. Like Charlotte, Lynsey, 29, was unaware she was a carrier of the bacteria and was not tested or given the antibiotics which may have saved her son.
"I'd never heard of it before," she said.
"We didn't understand how sick he was. Saturday and Sunday they tried their best.
"On Sunday night he had gone into multiple organ failure and he'd started having seizures. They said they'd try one more thing and if not we'd have to withdraw care.
"They did a brain scan and it showed damage, so they took us into a room and removed support and he died 20 minutes later in my arms on the Monday. It was very quick."

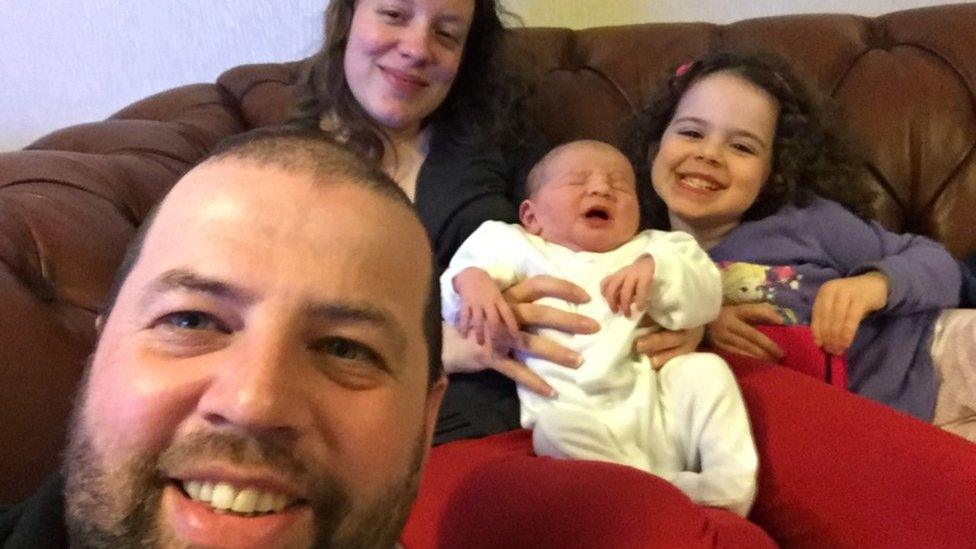
Craig White and Lynsey Dalvarez with their Frankie, who died after being born with the condition
Both Lynsey and Charlotte feel very strongly that every mother should be tested for the condition.
While this is done in some European countries and the US, routine screening is not done in the UK.
The decision on whether to introduce it in this country is down to the Department of Health, which takes expert advice from the National Screening Committee.
The screening committee is currently looking at this, but has said in the past that it does not think there is a case for routine screening here because it does not believe it is accurate enough.
Dr Anne Mackie, Director of Programmes for the UK National Screening Committee (UK NSC), said: "The UK independent expert screening committee's last review of screening for group B strep carriage found testing in late pregnancy unreliable.
"This is because the test cannot distinguish between women whose babies will be affected by early onset group B strep and those who would not. This could lead to a high number of mothers and babies being exposed to unnecessary antibiotic use."
'Trauma'
Campaigners disagree with the screening committee and say concerns about the overuse of antibiotics should not prevent mothers from being routinely screened.
Jane Plumb from the charity Group B Strep Support, said: "Screening will save babies' lives, stop families going through the trauma of seeing their baby suffer preventable infection and ease the burden on our overworked NHS."
They point to a clinical trial undertaken at London's Northwick Park Hospital in which more than 5,000 women were screened, with those testing positive offered antibiotics in labour.
Full trial results are expected to be detailed in the British Medical Journal soon but preliminary results given after the first 18 months showed an 80% reduction in the number of babies infected with the bacteria.
More than 250,000 people recently signed a petition calling on the Department of Health to introduce routine testing in the UK.
The Department of Health declined to comment until after the screening committee report, which is expected some time this month.
5 live Investigates is on BBC Radio 5 live, Sunday 5 March at 11:00 GMT - catch up on BBC iPlayer Radio.
Have you got something you want investigating? We want to hear from you. Email 5liveinvestigates@bbc.co.uk
- Published20 February 2013
- Published18 July 2016