What will medicine be able to do with hearts?
- Published
- comments
If heart transplantation - 50 years after Christiaan Barnard carried out the first operation - has become routine, what exactly will medicine be capable of in the future?
Will we one day be able to build, or even grow, replacement hearts, or will surgeons be able to use genetically modified animal hearts in their place?
The pace of progress has been staggering.
Harefield Hospital heart and lung transplantation director Mr Andre Simon says: "I fell into the trap when I was 18 and I saw my first heart transplant. That was 1986.
"There were two surgeons. I could see them tying knots, and you couldn't see their fingers because they were so fast. It was weird, fantastic.
"It was the end of the 'cowboy' time in cardiac surgery. I remember coming into the office, and I was impressed by the fact that everything was full of cigarette butts and empty beer bottles.
"It was a completely different time. Things have changed.
"Overall, we are in a lot better position because we can do things we couldn't do - but we have also lost some of the necessary will to push limits."
The operation that took medicine into the media age
Witness: The First Heart Transplant
New techniques are badly needed because the number of donor organs - about 200 per year in the UK - is dwarfed by demand. About 2,000 people under the age of 65 a year will die of heart failure without a transplant.
One option researchers hope to develop is to use stem cells to grow new cardiac muscle.
Dr Doris Taylor, director of the Center for Cell and Organ Biotechnology, at the Texas Heart Institute, in Houston, says: "If we want to build a whole heart, that takes hundreds of billions of cells.
"The good news is we can now do that.
"My goal is within the next six months to have two to three hearts built that are contracting at a level that makes them transplantable [into large animals such as cows]."
Using pigs, Dr Taylor's team are stripping cells from hearts, and then rebuilding them using stem cells.
They are hoping to perfect a technique where a diseased heart is plumbed up to a newly grown heart.
Ultimately, they hope the new heart can take over completely.
"What we have found is that cells that migrate to different areas tend to differentiate into the type of cell that belongs in the region in which they find themselves," Dr Taylor says.
However, cardiothoracic surgeon Prof John Dark warns against raising false hopes.
"One has seen people come up with very exciting ideas several times in the past," he says.
"Twenty years ago, we thought we were on the verge of taking organs from pigs and using them for so-called xenotransplants. And while there are some exciting developments in that field, we are still not there.
"Ten years ago, there was huge excitement about using stem cells to repair damaged hearts.
"The clinical results have been very disappointing: we have seen a few percentage points' improvement in the function of hearts in patients in large clinical trials.
"One wants to see the final product before you are really convinced."
Mechanical devices can help failing hearts
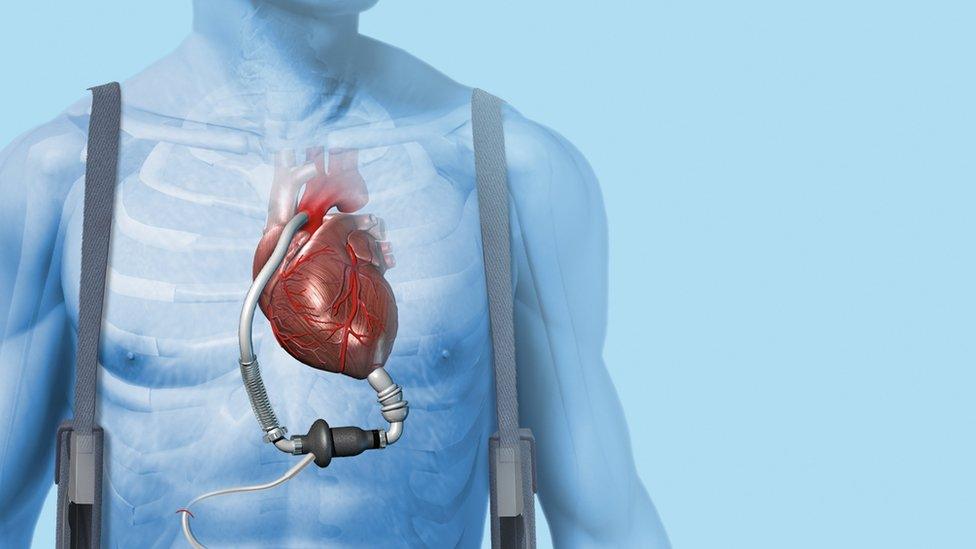
An alternative to growing new hearts is to refine devices that can keep a patient alive until they can have a transplant.
In recent years, the left ventricular assist device (LVAD) - an artificial pump that helps the left side of the heart do its job - has shrunk from a large external piece of kit to a tiny battery-operated device that can be implanted into the chest.
For the first year, they are as effective as a transplant.
Each generation has become more effective, but there is still a risk of infection, and they are not always easy to live with.
Will the next step be the development of mechanical hearts? Mr Simon thinks so.
"I can see that such a device, if mass produced, is not going to be that expensive," he says.
"It is going to be like a pacemaker, you just go and get one, like a new iPhone.
"The problems we face are making a device that does not lead to clotting and strokes, and works 100%."
Researchers are also working to try to preserve a heart for longer after it is removed from the donor.
At present, speed is of the essence to maximise the chances of success - more than three hours, and the odds decrease sharply.
The current technique is to stop the heart and store it in a cool solution.
But experiments have shown that if a beating heart is perfused with warm blood, it can be preserved for much longer out of the body - up to 12 hours.
Scientists hope that eventually it will be possible to store hearts for up to a month.
This would potentially enable hearts to be matched up immunologically to the patients most likely to benefit.
The key to the future is not likely to be any single technology, but a combination of all of them.
But if the past 50 years have taught us anything at all, it is that things that seem impossible today will become the medicine of tomorrow.
BBC Radio 4 is marking 50 years since the first heart transplant with a range of programmes this week. Dr Fong presents Inside Health Special: The Future Heart on Tuesday, 5 December, at 21:00 GMT.