Long A&E waits: 3m a year wait over four hours
- Published

The number of long A&E waits across the UK has more than doubled in the past four years as hospitals struggle to cope with demand, BBC analysis shows.
Northern Ireland has the worst performance, although England has seen the fastest deterioration, the figures show.
Over 3m patients who visited UK A&Es waited over four hours in the past 12 months - up by 120% since 2012-13.
By comparison the number of visits has only risen by just over 7% to 26.9m.
If you can't see the NHS Tracker, click or tap here, external.
Doctors and nurses said the findings showed the NHS could no longer cope with what was being asked of it and patients were being put at risk.
And Dr Taj Hassan, president of the Royal College of Emergency Medicine, said the A&E system had been "stretched to its very limits".
"Staff are working really hard. But we've reached a point where we cannot meet demand.
"Life-threatening cases are prioritised. But a crowded emergency department adds risk. We get delays to assessment, pain relief and antibiotics."
Royal College of Nursing general secretary Janet Davies agreed, describing the situation as "intolerable" and A&E units as "full to bursting".
"Nursing staff in A&E units have been telling us it's hard for them to do more than firefight," she added.


How far short is the NHS of the target?
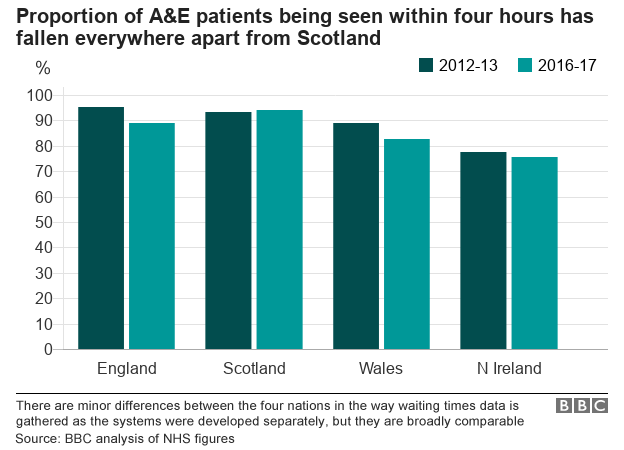
The data compiled by the BBC shows a significant difference in performance against the four-hour target for treating or admitting patients.
In Northern Ireland, which has seen the biggest rise in people coming to A&E units, just 75% of patients were seen in four hours in 2016-17, whereas Scotland saw 93.9% - only marginally lower than the 95% target.
In fact Scotland is the only part of the UK performing better than it was four years ago.
England has seen the biggest rise in long waiters - a 155% increase. In Scotland the number of long waiters actually fell by 9%.
Regionally in England the West Midlands has the worst performance followed by the North West - patients visiting A&Es in those areas are more than twice as likely to wait over four hours than those in the North East, the best-performing region.
There are minor variations in the way the target is measured across the four nations, although they are considered broadly comparable.
'You feel like you are failing patients'

The BBC has been speaking to a number of hospital staff this week about their experiences. Many wanted to remain anonymous given the political sensitivity about the performance of the health service.
But all agreed the pressures were as great as they had ever experienced. One nurse, who works in an A&E unit in south Wales, said his department faced relentless "24/7" pressure.
"I know of colleagues who leave a shift and then come back the next day and find the patient is still there. We have seen them in A&E but there are not beds in hospital. It causes overcrowding and all sorts of delays.
"Ambulances queue outside A&Es as the staff are too busy to take patients off them. I've worked in A&Es for over 10 years and this is as bad as I can remember."
Another nurse, from London, said: "You feel you are failing patients. This is not the sort of care we want to provide, or patients deserve.
"We obviously prioritise the most serious cases, but when it is this busy there is always a risk you miss something. I sometimes finish my shift and end up worrying about my patients."
Patients have also been contacting the BBC.
One of those was Hayley Hughes, who waited over five-and-a-half hours at an A&E unit in Wales after sustaining a head injury.
"I kept falling asleep, which worried my partner.
"There was another couple we were speaking to who had got to A&E about an hour before we did, and they were still waiting when we left. I'd say they were there for about six-and-a-half, maybe seven hours.
"It's ridiculous. Whilst I was being assessed you could see the strain on the faces of the staff."
Is there a solution?
Unless the NHS can get its existing network of hospitals to see patients more quickly, the health service would need another 20 A&Es staffed by at least 170 consultants to hit the target again.
But each nation believes the answer to the problem lies in trying to control the numbers turning up at A&E and ensuring they pass through hospital more quickly when they do need treatment by freeing up beds.
This is done by making sure there are spare beds in care homes and care services in the community, to hand over frail patients to.

In Scotland, for example, NHS budgets have been pooled with council funds to create a closer working relationship between hospitals and care in the community, which is one of the reasons why ministers there believe they have performed better than the rest of the UK.
In England an extra £1bn is being invested in social care this year, while £435m has been freed up to help with winter planning, including putting GPs in A&Es to deal with the more minor cases.
A Department of Health spokesman said ministers acknowledge the NHS was "under pressure due to the ageing population", but he pointed out that despite the deterioration, nine in 10 patients were still dealt with in four hours.
Chris Hopson, chief executive of NHS Providers, which represents hospitals, said the money had come too late.
"We are not where we would want to be as we head into winter. We cannot say with certainty how tough this winter will be, but the likelihood is that services will be sorely tested."
A spokesman for the Welsh Government said there were signs performance was improving when you compared this year to last year instead of four years ago.
But he admitted winter would be "challenging".