Stop prescribing 'precious' antibiotics for sore throats, GPs told
- Published
- comments

Doctors should not prescribe "precious" antibiotics for most people with sore throats and should recommend drugs like paracetamol, new guidelines say.
The National Institute for Health and Care Excellence said most sore throats were caused by viral infections, which cannot be treated by antibiotics.
But research suggests antibiotics are prescribed in 60% of sore throat cases., external
NICE said it was "vital" the medicines were only used when effective because of the rise of antibiotic resistance.
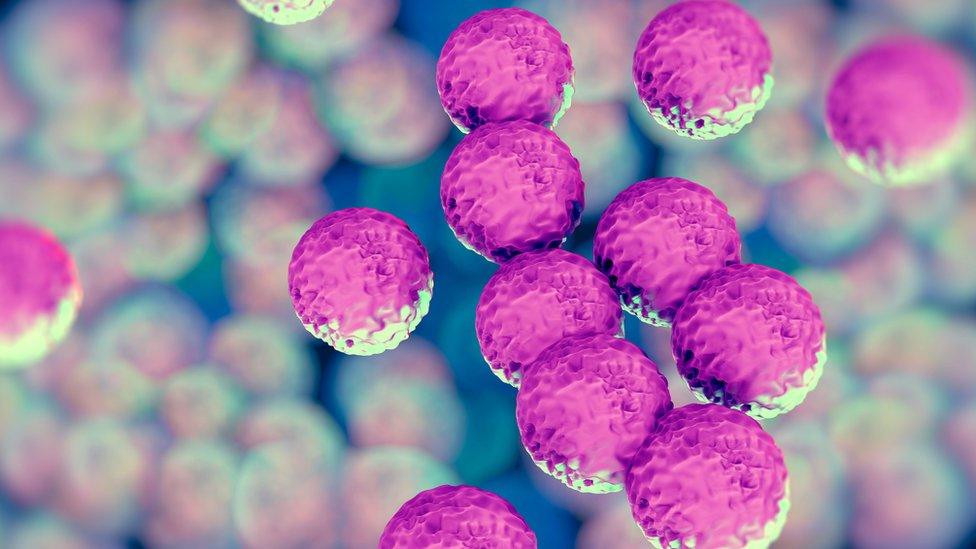
The overuse of antibiotics is making infections harder to treat by creating drug-resistant superbugs.
'Precious resource'
Acute sore throat, including pharyngitis and tonsillitis, can be caused by a bacterial or viral infection, with symptoms usually improving by themselves within a week.
New guidelines from NICE and Public Health England, which aim to limit the use of antibiotics, said doctors should only be prescribing the medicines for more severe cases that are likely to have been caused by a bacterial infection.
Most people should instead use pain relief drugs, which also include aspirin and ibuprofen, and certain throat lozenges, as well as drinking plenty of water and resting.
Prof Cliodna McNulty, head of PHE's primary care unit, said: "Antibiotics are a precious resource and it's important that they are only used when they are really needed.
"For a sore throat, evidence shows that antibiotics make little difference to length or severity of illness, unless symptoms are much more severe. While a sore throat can be painful, there are other ways to control the symptoms including taking paracetamol and medicated lozenges."
NICE and PHE also said doctors should use set criteria to judge how likely it is that people have sore throats caused by bacterial infections.
This works by checking people for scores across a range of symptoms, which include fever, pus on tonsils, severely inflamed tonsils and the absence of a cough.
'Post-antibiotic apocalypse'
England's chief medical officer, Dame Prof Sally Davies, has previously warned of a "post-antibiotic apocalypse" where infections would become harder to treat and common medical procedures such as cancer treatments could become too risky.
In some cases people have died from bugs that are resistant to all antibiotics.
In October, PHE said patients had "a part to play" in stopping the rise of infections and that more of them should be told to go home and rest rather than be given antibiotics.

In some cases people have died from bugs that are resistant to all antibiotics
Prof Gillian Leng, deputy chief executive at NICE, said people who needed antibiotics should be given them.
"But it is clear that routine prescribing in all cases isn't appropriate," she said.
"We are living in a world where bacteria are becoming resistant to antibiotics. It is vital these medicines are protected, and only used when they are effective."
The Royal College of General Practitioners, which supports the new guidelines, said patients needed to understand that antibiotics are "not a cure for every ill".
- Published23 October 2017

- Published27 October 2017