Could patients become their own doctors?
- Published

An NHS where patients stay at home and rarely attend GP surgeries or hospital out-patient appointments is likely in a decade's time, according to US health expert Dr Eric Topol, external, who was asked by ministers to look at how technology would change the role of health staff in England.
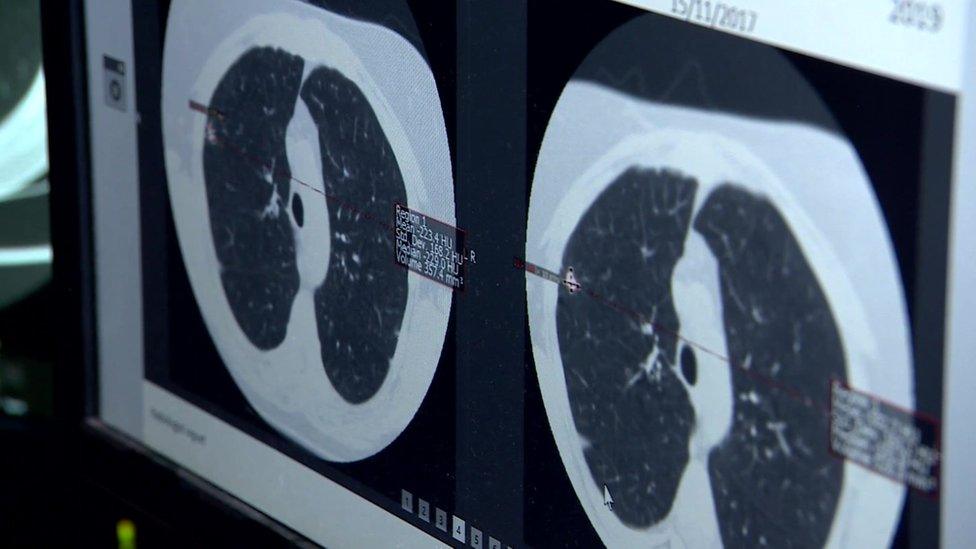
Many patients, according to his report, will be managing their own long-term conditions, for example high blood pressure and lung disease, with wearable devices and sensors, which will be much more effective than occasional appointments with a doctor.
The buzz phrase is the "democratisation of healthcare".
People who might have had to occupy a hospital bed for a few days for observation will be sent home instead.
Elderly patients, including those with dementia, will be monitored at home, with cameras and devices to detect falls built into the floor.
Fewer doctors
A new army of healthcare professionals is set to emerge to help technology-empowered patients.
This will include nursing associates, working alongside registered nurses and trained to interpret blood pressure and temperature checks.
Likewise, more physician associates will support doctors with the diagnosis and management of patients.
Fewer doctors than anticipated will be needed, under this vision of the future, and they will be able to focus on the sickest patients and avoid the risk of burnout caused by an excessive workload.
Better diagnosis
NHS England has already announced a plan to cut the number of out-patients' appointments and encourage remote monitoring and consultations.
The Topol report gives the example of fracture clinics and notes that at Brighton and Sussex University Hospital Trust trained therapists deal with patients over the phone and most are not seen in person, meaning consultants can review them within 72 hours of referral.
No serious complications for patients have been reported.

Dr Topol says the NHS, as an efficient, proven system delivering healthcare for the whole population, is well placed to take advantage of new medical technology and the UK is already leading the world in genomics (the study of an individual's genes), which allows better diagnosis and more personalised care.
Personalised service
Welcoming the report, the Health and Social Care Secretary, Matt Hancock, said technology saved lives and opportunities had to be seized - but when it came to sophisticated technology, the NHS was lagging behind Tesco.
"They know who you are through loyalty cards, where you shop, through store IDs, what you buy, the items scanned at the checkout," he said.
"They shape their offers with a personalised service in order to deliver for you, the customer.
"The NHS doesn't have anything like that yet."
It still did not have the data to determine which hospitals patients had been to and what medicines they were taking, Mr Hancock added.
Financial incentive
Sceptics will say this needs money and the NHS in England already has multiple calls on the funding allocated by the government.
Danny Mortimer, chief executive of NHS Employers, said: "The deployment of technology will of course require significant resource and investment and we would repeat that this needs to be properly funded by government and not left to already stretched individual NHS trusts to dig even deeper to fund."
On the other hand, the NHS has a powerful financial incentive to adopt the Topol vision.
More patient care in the home in theory means less need for expensive overnight stays in hospital.
Telemedicine means consultants can get through longer lists of patients, using video or phone consultations.
The challenge is to ensure the drive for efficiency does not over-ride the need for human interaction between doctor and patient when required.
- Published20 July 2018
- Published2 January 2018
- Published13 August 2018