Bereaved father leads NHS movement against suicide
- Published
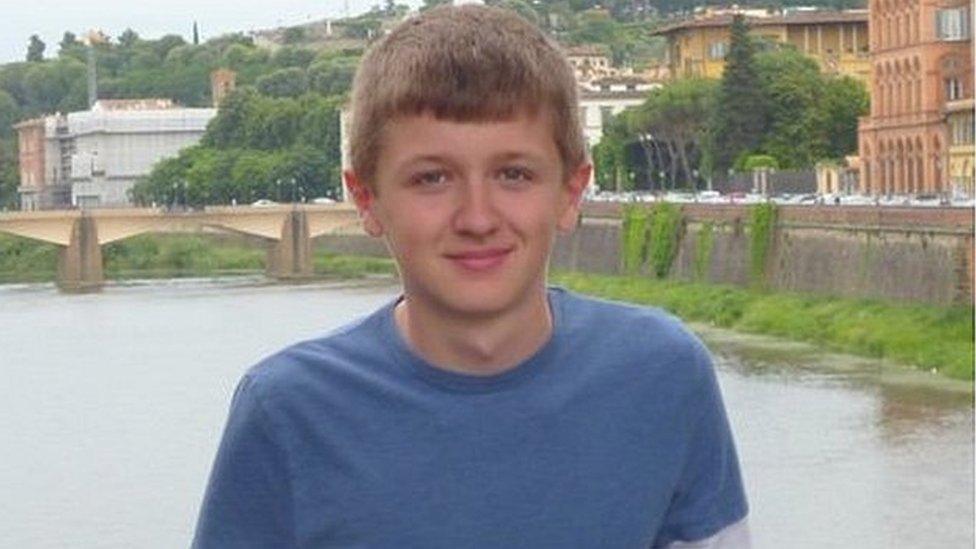
Edward Mallen killed himself shortly after his 18th birthday
It has been a painful journey for Steve Mallen, whose 18-year-old son killed himself in 2015.
Edward Mallen was a talented student who had won a place at Cambridge University.
The inquest into his death found he had "slipped through the cracks" of local NHS mental health services.
At Edward's funeral, his father vowed to investigate what had happened and fight for reform to prevent other deaths.
That vow has turned into a remarkable personal campaign, culminating with the foundation and launch of a movement across the NHS, the Zero Suicide Alliance, external.
One hundred and fifty hospitals, mental health providers and local health commissioners in England have joined the initiative.
They have signed up to moves to "radically improve the experience of all those entering the health system with psychological trauma, whilst simultaneously upgrading front-line services to reduce misery, save lives and produce better clinical outcomes".
Training one million people in awareness of suicide and prevention is one of the key aims.
Mr Mallen has reached this point by banging on doors in Whitehall and around the NHS - and, by his own admission, making a nuisance of himself.
He has refused to be brushed off and has insisted on building up a grassroots movement rather than relying on top-down ministerial edicts.
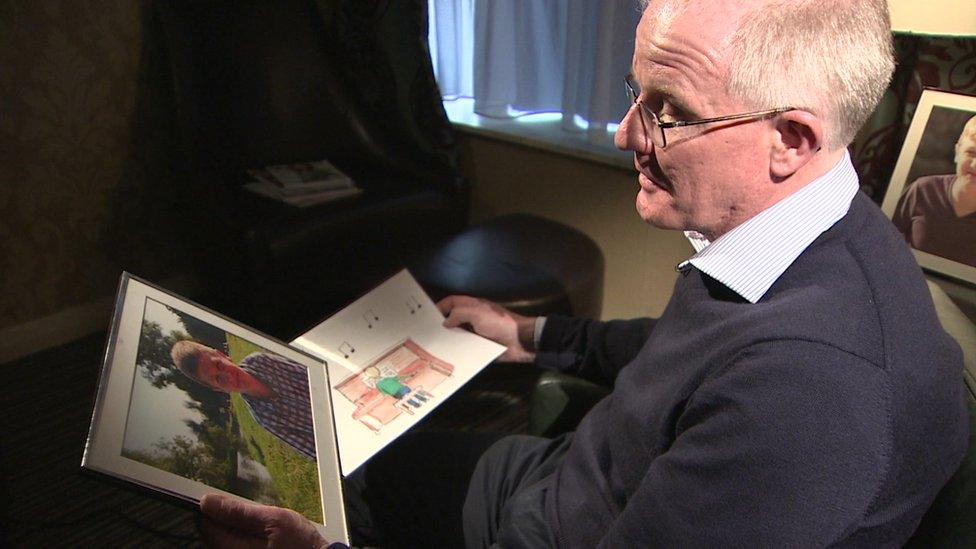
Steve Mallen vowed to investigate how the system had failed his son
In one sense, this is a unique development - with NHS organisations taking the lead and national health leaders coming on board later.
Mr Mallen said: "In honour of my dear son and the thousands we have lost so needlessly to suicide, together with the hundreds of thousands who are suffering from mental illness today, we are pleased to be launching a new model and a new vision for mental healthcare and suicide prevention.
"We have set ourselves the bold target of reforming the whole system."
Remarkable results
Alongside Mr Mallen is Joe Rafferty, the chief executive of a pioneering mental health trust, Mersey Care.
This was one of the first to adopt a Zero Suicide policy, external.
Recognising that 27% of the people who killed themselves were under the care of a specialist mental health team, Mersey Care set out to eliminate suicide among its patients.
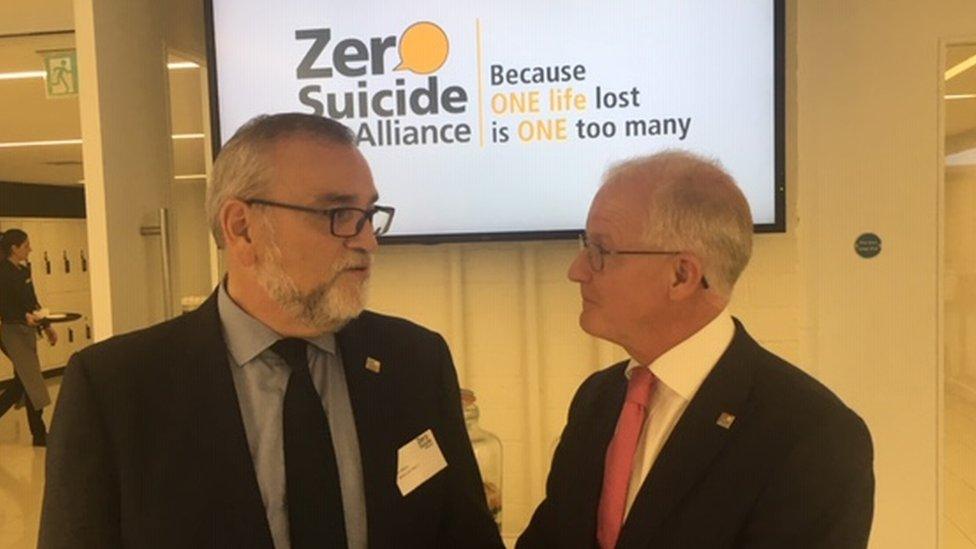
Joe Rafferty and Steve Mallen are working together
Staff training was central to the action plan. The result has been a reduction in suicides by more than a quarter since 2015.
The third founder member of the alliance was Geraldine Strathdee, formerly NHS England's national clinical director for mental health.
Together, they called on their network of contacts to persuade other health trusts to sign up.
They acknowledge that eradicating suicide will be impossible but they want organisations looking after patients and, beyond the NHS, employers with a duty of care to staff to at least try.
Ministers have willingly offered backing and the government has committed £2m over two years to support the initiative.
Jackie Doyle-Price, the first to have the title Suicide Prevention Minister, spoke at the first conference organised by the alliance.
She said her job was "to tackle the whole of government" on suicide prevention, which was "everyone's business".
Growing problem
She said staff on the rail network had been trained for interventions that could save lives.
And, noting that a third of suicides were outside the home, she explained how staff at agencies running public places were also being made aware of suicide prevention.
Mr Mallen and his co-founders have come a long way in a short time but they know they have some way to go.
According to the Samaritans, suicide rates among young people have been rising even though there has been a decline across the whole population.
On BBC Radio 4's Today programme, Mr Mallen spoke of the need for more open conversations between the NHS, patients and their families about feelings and suicidal thoughts.
"My son would still be alive if we had those conversations," he said.
"If I could turn back the clock, which is what we are seeking to do with this alliance, he would still be here."