Painkillers 'mask, not kill' long-term pain
- Published

Jazz is using exercise to help her recovery
Excessive use of painkillers is on the rise. Now the NHS in Sunderland, which has one of the highest prescribing rates, external, is running a campaign to raise awareness of the dangers of long-term use.
Jazmine Allen, 23, who already has a 10-year history of using prescription painkillers, is taking part in the 'Painkillers Don't Exist', external campaign - which aims to raise awareness that the medications can simply be masking the pain rather than "killing" it - and encouraging patients to seek support from their GPs.
Jazz began taking opioids as a teenager, after surgery for hip dysplasia brought her serious, chronic pain.
But when she went to university, she realised the pain medication was becoming more of a problem than the pain itself. And it was consuming her life.
"I was a child. I was put on this through no fault of my own, and coming off it was a million times harder than any of the surgery stuff", she says.
"I was so tired and drained and I was so dependent on them."
Her GP suggested she went to a drug and alcohol rehabilitation centre in Leeds, which dealt with people coming off high-dose opioids for methadone to help her come off her prescribed medication.
But she decided it was "ridiculous, treating an opioid with an opioid". She opted to come off her painkillers, and uses exercise to manage her symptoms instead.
'North-South divide'
At the University of Manchester, a team has been studying the increasing prevalence of painkiller use.
Dr Li-Chia Chen has been looking at opioids, and more recently the rise of gabapentin and pregabalin (medications used to treat nerve pain).
Her findings on both show a similar picture - that the poorest communities have the highest dependency on pain relief.
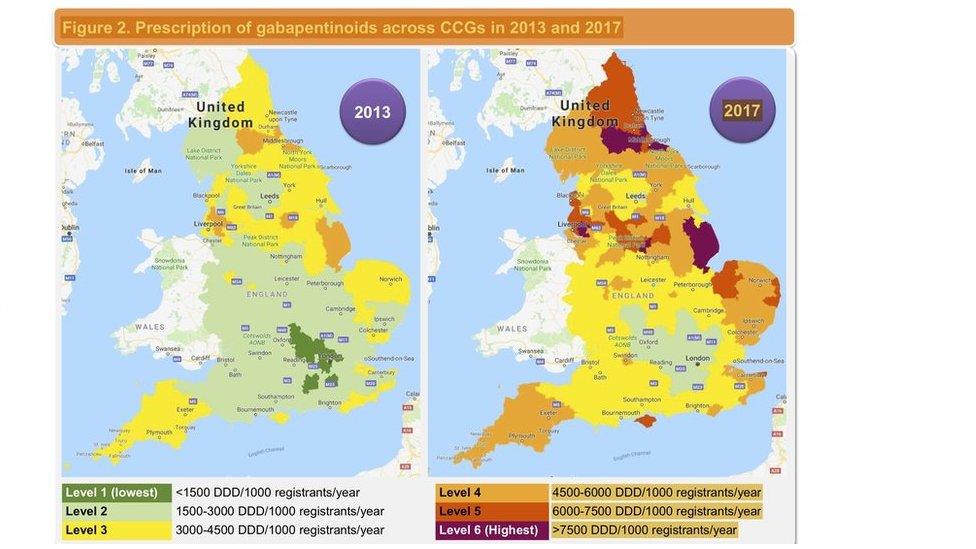
Prescriptions for gabapentin and pregabalin have risen steadily over the last decade.
"There is a very clear North/South divide" she says.
"In more deprived areas there are more people in labour-work type of jobs. They may damage themselves so they have more muscular skeleton conditions, and lower back pain.
"But the other thing is how they access their healthcare, so maybe healthcare demand is high but healthcare provision is not sufficient to care for those patients."
Public Health England data, published last year, showed 540,000 people in England have been taking opioids, gabapentinoids or benzodiazepines for three years or more, risking overdose and dependence.
Doctors know painkillers can be of huge benefits to some patients. Research suggests just one in 10 patients seeking help for long-term pain, benefit from strong painkillers.
'Is something else going on?'
But Dr Siara Malik, who is helping run the Sunderland campaign, says they're working hard to reduce long-term use.
"We need, as clinicians, to be chasing up our patients to see why the pain is persisting.
"For patients to be aware if they are taking if for that long, they need to be asking why am I taking it, is there something else going on, is it masking a problem that needs further attention?"
NHS Sunderland is running a campaign aimed at long-term users of painkillers
Following the Public Health England report, external, the All-Party Parliamentary Group for prescribed drug dependence called for a national 24-hour helpline providing withdrawal support, tapering, and drug information for patients, their families and doctors.
They have also recommended dedicated withdrawal support services working with GP surgeries to help identify patients, and provide advice and support, as well as better provision of alternatives to pain killers.
Prof Peter Kinderman, who is on the group, says action is needed now.
"There is general acceptance we have a problem, I think we also agree on what the solutions are. The real next step is government implements the recommendations rather than say there is a problem."
NHS England and NHS Improvement are considering the recommendations from the review, including the recommendation for a helpline.
The government stresses painkillers are essential to help people manage pain, but they must be treated with caution.
It continues to support a range of evidence-based approaches to reduce prescribed medication dependency, including the recent introduction of addiction warnings on the packaging of opioid painkillers.
- Published6 February 2020

- Published16 January 2020

- Published10 September 2019
