Am I helping to protect the NHS?

Remember life before the lockdown? This is Angie.

Like many of us, she was going to work, seeing friends and family.

But what she didn't know was that she had contracted the new coronavirus, which causes Covid-19.
Before she developed any symptoms, she had passed the virus on to her friends Mikah and Steph, as well as her grandad Terry.
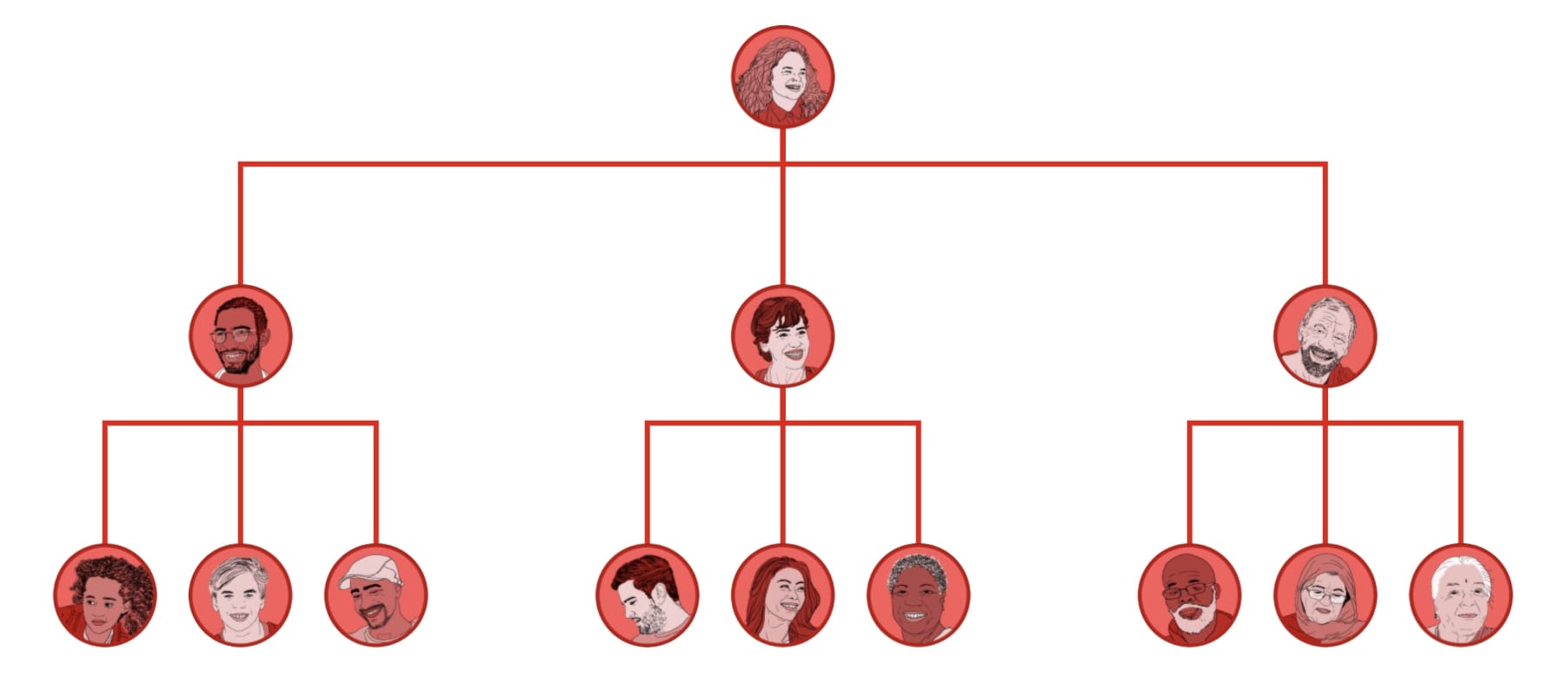
Each of them then went on to meet their own friends and family.
On average, without social distancing in place, scientific modelling suggests that people infected with coronavirus would pass it on to another three people.
For this reason, among Angie's network, cases multiplied and spread quickly - soon extending far beyond her original community.
Although most of these people who contracted the virus would experience either mild symptoms or something like a nasty flu and make a full recovery, some would require hospital treatment.
According to scientific modelling by Imperial College London, about 4.5% of those infected would need to be admitted to hospital - shown here as 100 dots.
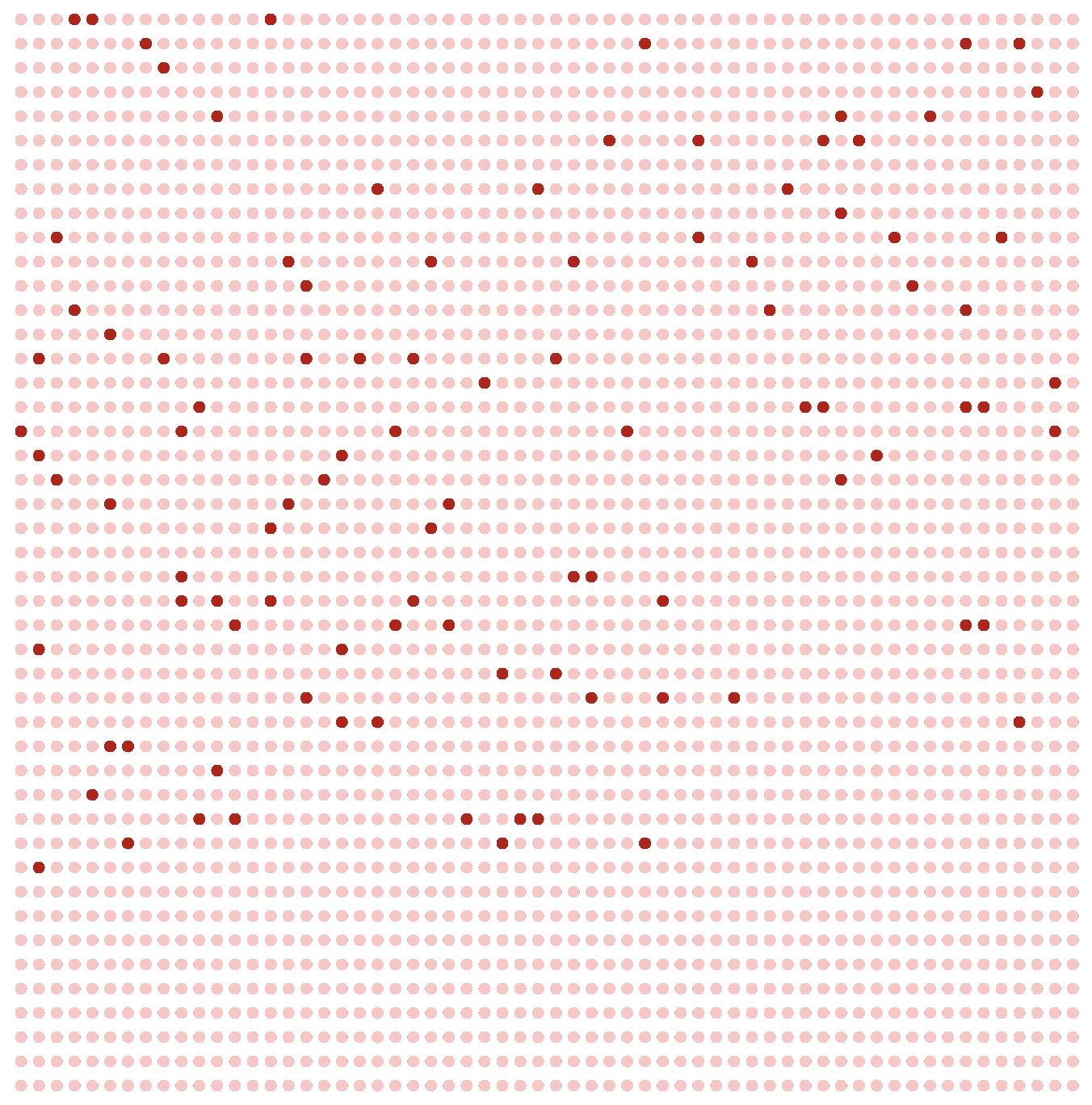
The Imperial modelling also predicts that out of the 100 people needing hospital treatment, about 30 would need a critical-care bed.
But the problem the NHS has been facing is that for each group of 30 patients in need of a critical-care bed, there would be just one such bed available when the epidemic reached its peak.


This would mean NHS doctors facing impossible choices about who receives potentially life-saving treatment, and who doesn't.

For example, should Mathilda, a retired teacher and 78-year-old grandmother-of-seven get the bed?

Or Hamish, a 68-year-old ex-firefighter and the sole carer of his wife Philippa, who has Alzheimer's disease?
To prevent doctors having to face these dilemmas, the Imperial team assessed different ways of reducing the number of people needing the NHS's critical-care beds.
They found that if people experiencing symptoms, and everyone who lived with them, stayed at home for two weeks, while anyone over 70 reduced their social contacts to a minimum, the impact on the NHS would be reduced. This is similar to the measures the UK government introduced before the lockdown.
But there would still be about eight patients for each critical-care bed available. The NHS would still be overwhelmed.
The Imperial team also found that if social distancing measures were applied to all age groups - not just to those over 70 - schools and universities were closed, and the two-week quarantine period applied to households in which any member had symptoms, the NHS would be able to cope.

However, in places where demand happened to be above average, NHS services would still be under extraordinary pressure.
This Imperial College research has been very influential and the above approach is similar to what UK government ministers have since implemented. So far the NHS has not been overwhelmed largely because of social distancing and lockdown measures.
But there's a major catch.
As soon as the current measures are lifted, the Imperial model predicts that another outbreak would emerge that was just as bad as if we had done nothing.
Although the research was published on 16 March, its core message is still current: Prime Minister Boris Johnson warned on Monday that lifting the lockdown too soon could result in a second wave of infections.
The only two ways out of lockdown are the development of a vaccine or a much more effective system of testing people for the virus and tracing all those who had contact with people testing positive, potentially via the NHS app now in development.
There are many assumptions in the Imperial College model about how the virus is transmitted, and what proportion of people will comply with the restrictions now being placed on them.
Since the Imperial research was made public, there has been a huge effort by ministers and NHS officials to increase the number of critical-care beds available - up from the 5,000 or so that the NHS had at that time.
But what is clear is that the biggest impact individuals can have on the final toll in the UK is to reduce the rate of transmission by following the latest social distancing guidelines: working from home if possible and only going out for essential reasons and daily exercise.



 Coronavirus: Boris Johnson fears second peak from relaxing lockdown
Coronavirus: Boris Johnson fears second peak from relaxing lockdown