'Thousands missing out on cancer diagnosis'
- Published

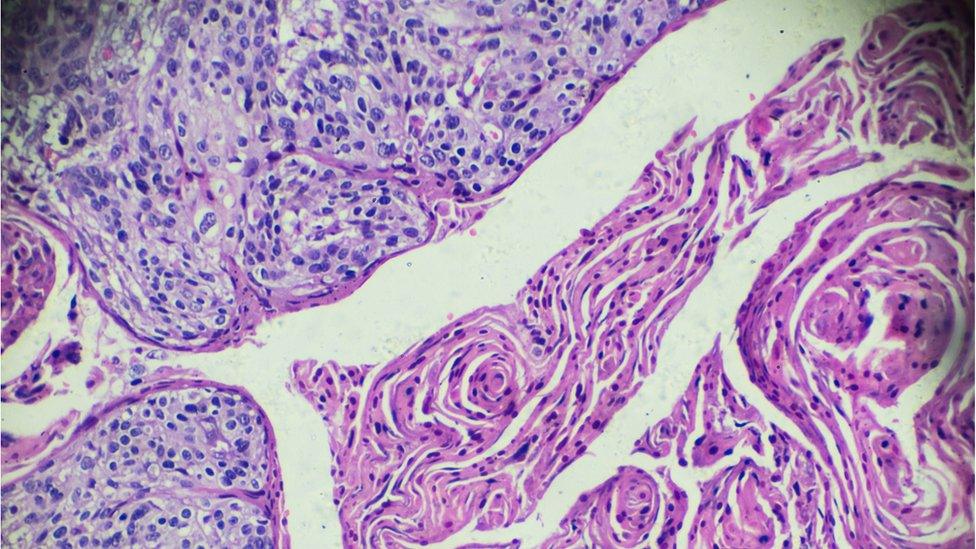
Breast screening is just one of many ways of picking up cancers
Delays in diagnosing and treating people with cancer could lead to more years of lost life than with Covid-19, according to a leading cancer expert.
A drop-off in screening and referrals means roughly 2,700 fewer people are being diagnosed every week, Cancer Research UK says.
Cancer screening has paused in Wales, Scotland and Northern Ireland, with few invitations sent out in England.
People are still advised to contact their GP with worrying symptoms.
But Richard Sullivan, professor of cancer and global health at King's College London, said there was more fear of Covid-19 than of having cancer at the moment. With GPs more difficult to contact than normal, this was resulting in a "dramatic drop-off" in referrals to specialists, he said.
"Most modellers in the UK estimate excess of deaths is going to be way greater than we are going to see with Covid-19," he said.
With cancer patients generally much younger, Prof Sullivan predicted "years of lost life will be quite dramatic" on top of "a huge amount of avoidable mortality".
'I don't know if my cancer has spread'

Maggs Bailey doesn't know if her skin cancer has spread because of a cancelled appointment
Maggs Bailey, 58, from Reading, had a mole removed last year and found out it was melanoma (a type of skin cancer) in February. She had another appointment in April to find out if her cancer had spread.
But she was "really upset" to find out it had been cancelled and no one had contacted her to say so.
"I sort of swing between feeling completely positive... to thinking 'oh my god I've got cancer cells running through my body and who knows what they're doing'."
Maggs says she completely understands that the NHS is under immense pressure with coronavirus, but wonders if the right decisions are being made. She is now considering private surgery.
"To be not able to have the treatment I feel I should be getting - I didn't really have any choice but to do something else about that. It's scary."

Sarah Woolnough, executive director for policy at Cancer Research UK, said it was of "huge concern" that there had been a 75% drop in urgent referrals by GPs of people with suspected cancer, external.
According to the cancer charity:
2,300 people a week are not being diagnosed through urgent referrals
400 people a week are not being diagnosed through screening
"Our plea is that we get back to some kind of normality as soon as possible," she said.
"Most screening hubs are not sending out invitations. Even though we have not had official word, screening is effectively paused in England. Patients are not seeking help and then if they are referred on, much of the diagnostic activity is on hold."
With a large number of staff self-isolating at home, many cancer treatments like chemotherapy and radiotherapy have been delayed.
"A lot of services have had to scale back - we've seen a dramatic decrease in the amount of elective cancer surgery," Prof Sullivan said.
He said huge numbers of patients would be stuck in a backlog when cancer services were opened up again, creating "an enormous challenge for hospitals".
It could take six to 12 months for cancer services to return to normal - but only if the lockdown measures were unlocked "very quickly", he said.
In the Commons, Health Secretary Matt Hancock said it was not advisable for some cancer treatments to go ahead during an epidemic, because of the risks of exposure to the virus.
'Lasting impact'
Peter Johnson, NHS clinical director for cancer, said: "Although the NHS is working day and night to tackle coronavirus, it is also open for business in other vital areas such as cancer diagnosis and treatment - if you have worrying symptoms, you should still contact your GP and be referred for further checks."
"It's vital that we have a safety net in place for people whose diagnosis and treatment is delayed, so that when we come through the other side of the pandemic, they can be prioritised as a matter of urgency," said Bowel Cancer UK chief executive Genevieve Edwards.
She said decisions taken now would undoubtedly have "a lasting impact" for some bowel cancer patients.
Rebecca Shoosmith, from Jo's Cervical Cancer Trust, said: "Dealing with changes can be extremely difficult and the support offered by charities can be a lifeline at this time.
"Safety netting by care providers is essential to ensure everyone facing cancellations or changes receives the care they need as soon as they possibly can."
- Published13 April 2020
