Covid: The things we’re not being told as lockdown looms
- Published
- comments
Lockdown 2.0 is on its way, with ministers saying they have been left with no choice if lives are to be saved and the NHS is not to be overwhelmed.
It seems to be an open-and-shut case. But as MPs prepare to vote on the lockdown a number of questions remain to be answered.
How will it be used to fix Test and Trace?
One of the benefits of lockdown, it has been suggested, is that it will provide time to fix England's NHS Test and Trace system.
It is routinely failing to meet its targets to reach people who test positive, and then obtain and contact their close contacts to ask them to isolate.
But solving that is easier said than done.

Councils are now being encouraged to set up their own local contact-tracing teams to try to improve the reach of the service.
About one-third have something up and running, but most are just at the start with skeleton teams and IT struggles.
Directors of public health are frustrated they were only given money to do this as the second wave got under way, rather than earlier in the year when infection rates were lower and it would have been easier to build up.
What is more, very few people appear to be isolating. Research suggests fewer than one in five are doing so fully.
The government is now providing help - those on low incomes are getting £500 support payments. But that, some say, is not enough.
"The government simply doesn't understand the difficulties people face in terms of lost income and job insecurity," says one chief executive who has had in-depth negotiations with the government on the issue.
"We're doing all this work to try to reach them, but then don't help them isolate. What's the point?"
Exactly how close is the NHS to being overwhelmed?
The government presents detailed statistics on Covid. They show more than 9,000 patients are currently in hospitals in England.
But what we are not being told is exactly just how full hospitals are.
The Covid patients take up fewer than one in 10 beds.
So far, both NHS England and the Department of Health and Social Care have refused to reveal the number of available beds once you take into account patients being treated in hospital for other conditions.
Figures obtained by the Health Service Journal, which the BBC understands are correct, suggest just over 80% of beds are occupied.
That's actually a little bit lower than it was last winter, reflecting the fact that despite efforts to do more non-Covid work, such as cancer care and routine surgery, the numbers remain well below pre-pandemic levels.
It provides a bit of wriggle room, but not much. In fact, those areas like Manchester and Liverpool that have seen a significant proportion of the admissions are close to being full.

But there are a number of options the NHS has to increase capacity. One is to start cancelling non-urgent treatments - and some hospitals have already started to do this.
The other is to use the Nightingale field hospitals. The one in the North West has started taking non-Covid patients to ease the pressure on hospitals in that region.
Could the others be deployed? Possibly, although unions have questioned where the staff are going to come from to care for patients.
But regardless of that it is virtually impossible to assess just how acute the pressures are.
NHS leaders are due to hold a press briefing on Wednesday, which may shed some light on the issue.
Why has more not been done to protect the vulnerable?
We know the virus has killed a disproportionate number of people who are either elderly or have an underlying health condition.
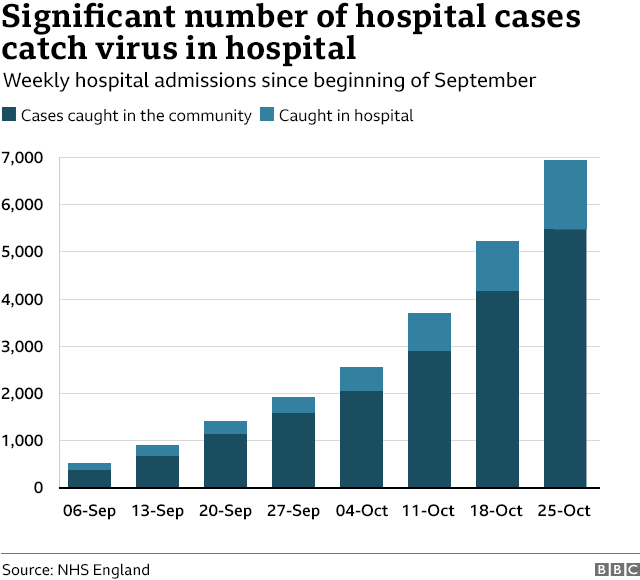
Yet as the second wave has taken off, the number of outbreaks linked to care homes has started increasing, while one in five of the "new hospital cases" are actually people thought to have caught the virus in hospital.
This is a source of frustration for many experts.
Research shows that three-quarters of deaths in the first wave came from just 5% of the population judged to be at highest risk, according to modelling by Oxford University.
This 5% will include people in care homes and those sick enough to be in hospital for other conditions.
Prof Mark Woolhouse, an infectious diseases expert at Edinburgh University, says he cannot understand why more is not being done alongside the social distancing rules already in place to protect such groups.
It could, he believes, "make a significant difference" to the number of deaths. "It's unconscionable we are not doing more."
What could be done? A range of different suggestions have been put forward to government.
These include supporting multi-generational households by offering free hotel accommodation, boosting the care home workforce so staff do not need to work across multiple homes making it easier for infections to spread, and providing more testing to hospital staff and also those who having caring responsibilities.
How many people could actually die?
One of the most alarming charts presented by the government when it announced the latest lockdown on Saturday looked at a range of scenarios for the number of predicted deaths in England.
The worst projection suggested deaths could reach 4,000 a day - as the graph below shows.

But it now turns out that projection was out-of-date.
It was based on figures from the start of October, which show by now there should be 1,000 deaths a day. The current average is a quarter of that number.
What is more, the Public Health England and the Cambridge University team that produced it have since published reports based on the more recently available data.
Grilled by MPs on this on Tuesday, chief scientific adviser Sir Patrick Vallance said he apologised if it caused confusion.
Could the second wave have peaked?
What is also interesting is that none of the scenarios for deaths factored in the regional restrictions that the government has imposed since mid-October.
The UK's chief medical adviser Prof Chris Whitty was pressed on this by MPs on Tuesday. He argued while there were some signs the restrictions were starting to have an impact, it would not be enough to get infections down sufficiently.


But others question this. Prof Carl Heneghan, director of the Centre for Evidence-based Medicine at Oxford University, says he is concerned by the use of clearly out-of-date modelling.
He says making such predictions is notoriously difficult and any forecasts "beyond two weeks" come with a huge margin of error.
There is, he believes, some signs the rise in infections and in hospital cases is beginning to slow and would like to see that given time to play out.
Prof Tim Spector, who leads the Covid Symptom Study, has gone even further, tweeting the peak of the second wave may have passed.
But he said this would take one to two weeks to translate to hospital infections and four weeks to change the trend on deaths.
What is the impact of lockdown?

The development of government policy is normally accompanied by a full assessment, comparing the benefit of doing something and balancing that against the cost.
When the UK first entered lockdown, this was not done.
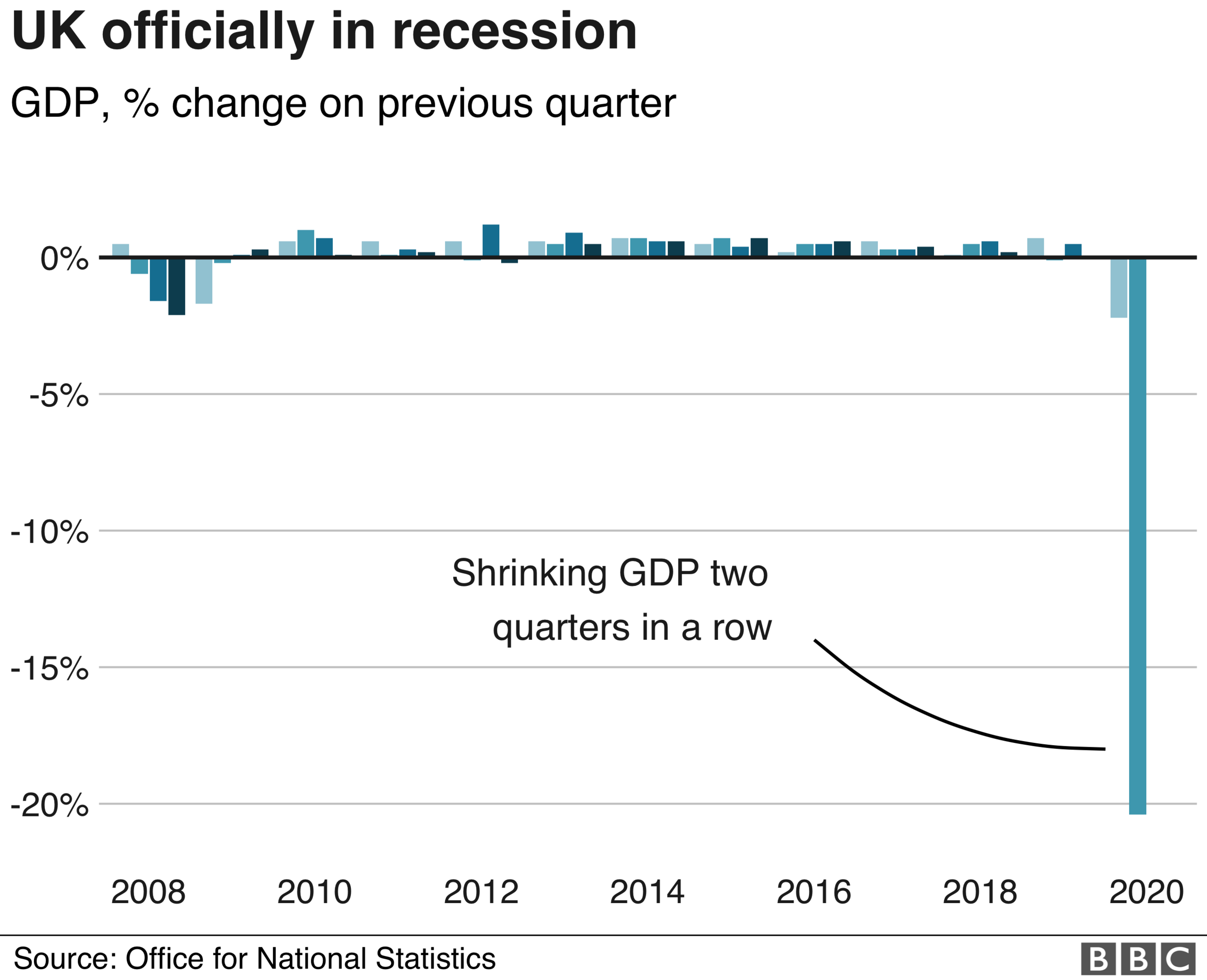
And that seems to have been repeated again despite warnings about the indirect toll of lockdown - from mental health problems and people delaying seeking help for other health conditions, to the economic consequences.
Although Sir Graham Brady, chairman of the 1922 Committee of backbench Tory MPs, has challenged the prime minister to publish the assessment if one is available before MPs vote later.

The government though says it is making attempts to minimise the consequences, pointing to the extension of furlough payments so employers can claim up to 80% of staff wages.
And it has been at pains to stress the NHS is still there for non-Covid health issues. In fact, it says without lockdown other services would have to be cut back because of the rise in Covid cases.
But the fear is lockdown will act as a deterrent to those seeking care, while isolation and job worries will increase mental health problems.
University College London psychiatrist Prof Sonia Johnson is worried that there has been "little specific focus on the costs of lockdown on the most marginalised and excluded" in society.
The risk is that the cure is worse than the disease - and some believe we are not properly modelling this to help work out ahead of time if it is.

LOCKDOWN LOOK-UP: The rules in your area
SOCIAL DISTANCING: How have rules on meeting friends changed?
SUPPORT BUBBLES: What are they and who can be in yours?
FACE MASKS: When do I need to wear one?
TESTING: How do I get a virus test?

- Published28 July 2020

