Covid: Does the NHS really need protecting?
- Published

England has exited lockdown but for nearly all the country, Wednesday marks just a small step back towards normality.
With the exception of Cornwall, the Isle of Wight and Isles of Scilly, strict restrictions mean people's lives are being curtailed.
A crucial factor - ministers have argued - is that the NHS risks being overwhelmed without the tough curbs on freedoms. But is this really true?
There are nearly 13,000 beds free
A quick glance at the latest data on hospital beds shows there were nearly 13,000 beds free at the end of November.
That's 50% more than last winter.


There are also several thousand beds available in private hospitals that the NHS has paid for until the end of the year that could be used for non-Covid patients.
It means, in theory, there are enough beds available to cope with a doubling of Covid patients - there are currently about 14,000 in hospital.
But that's just theory…
In practice, the NHS is meant to keep at least a tenth of its beds free to create flexibility to admit patients and cope with surges in demand.
It also allows time for cleaning and infection control - something that is, of course, particularly important during a pandemic.
In fact, the need for social distancing and infection control has meant hospitals have had to be reconfigured significantly, leading to 13,000 beds being lost from the system.


What is more, the pressures are not felt evenly around the country.
The past few months have been marked by individual hospitals getting dangerously close to full, with some reporting more than a quarter of beds occupied by Covid patients.
But the flip side of that is that some are not. Explaining why he was voting against the new tiers, Tim Loughton, the Tory MP for East Worthing and Shoreham, said his hospital had just four Covid patients.
These differences matter. Hospital capacity is one of the five key tests for working out which tier local areas are in.
Hospitals are trying to keep core stuff going
While doing this, the NHS is playing a juggling act. In the spring, a lot of planned work, including some cancer care, was cancelled.
The decision was taken because of the fear that hospitals could be completely overwhelmed. But it meant significant numbers of beds were left unused as the data for June in the chart below shows.


But this chart also demonstrates how the NHS has tried to get services back to normal over the summer and autumn with the number of non-Covid patients in hospital (shown in green) climbing.
This is deemed essential because of the growing backlog in numbers waiting for treatment. Macmillan estimates there are more than 40,000 missing cancer patients.
Meanwhile, the numbers waiting over a year for routine treatment, such as knee and hip operations, is at its highest level since 2008.
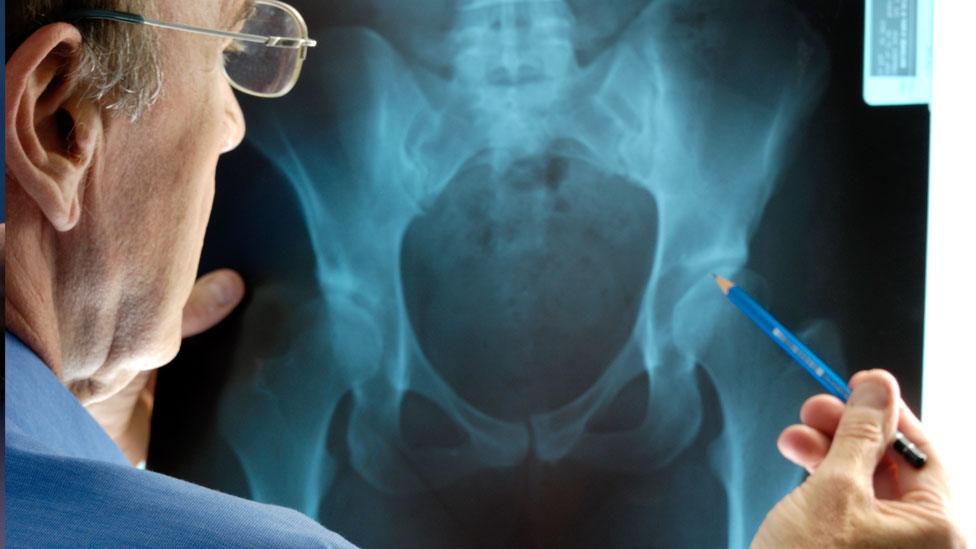
It is easy to think these sort of treatments can wait. But as Royal College of Surgeons of England president Prof Neil Mortensen says, these are patients whose lives are on hold left waiting "potentially in pain".
The desire to keep the non-Covid work going is strong - and when you put this all together, it leaves very little wriggle room.
It means any significant increase in Covid patients above the level seen now has a direct impact on non-Covid care.
All this is being done while staff are exhausted with significant numbers - 30,000 at last count - off work for Covid-related issues.
But what about the Nightingales?
England has a network of seven field hospitals known as Nightingales. These were built during the spring, again on the assumption that hospitals could become overwhelmed.
One of the challenges the NHS has faced is that it has fewer doctors, nurses and beds per head of population than many other western European countries.


Tory MP John Redwood has been vocal in calling for the Nightingales to be used, accusing those making dire warnings of trying to "scare" the public. Between them they could provide care to several thousand patients.
But the problem is they need staff. Chris Hopson, of NHS Providers, which represents hospital managers, says they were only ever built as an "insurance policy" to be used as a last resort if hospitals were overwhelmed.
To open them would mean spreading staff more thinly across hospitals and the Nightingales. That, of course, has consequences for the quality of care. It is the reason why only two have been pressed into action during the second wave.
Stretching the NHS beyond the point it is at currently is certainly possible, but it will have consequences.
Follow Nick on Twitter, external
Related topics
- Published11 November 2020

- Published5 July 2023

- Published5 July 2022

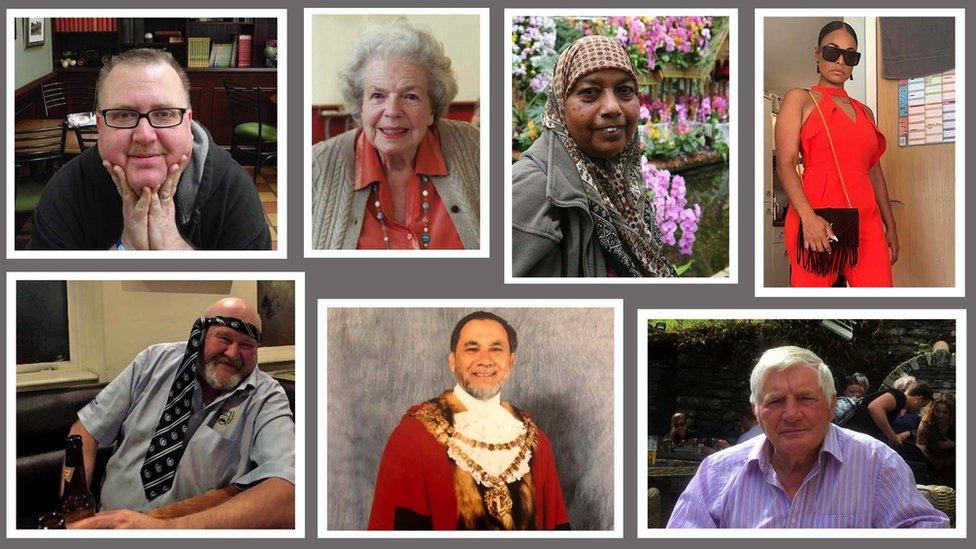
- Published30 April 2020