Covid vaccines: Why a giant plastic bag shortage is slowing the rollout
- Published
Although Covid-19 vaccine production has been ramped up from zero to billions of doses in record time, a shortage of raw materials and equipment has limited the number of doses that can be made.
To try to ease some of these bottlenecks, a marketplace has been launched, external - a sort-of pharmaceutical equivalent of eBay - to help manufacturers and suppliers see what is available and allow them to trade in one place.
The platform will help match unused materials and surplus stock to companies that need them, starting with the things under greatest pressure.
Here we take a look at some of the key components causing bottlenecks, as well as wider issues surrounding the rollout, such as intellectual property.
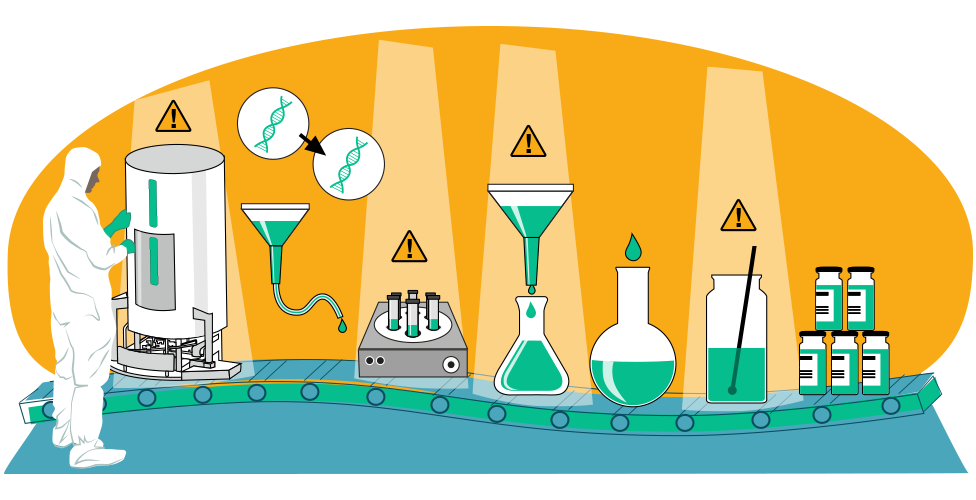
1. Giant plastic bags
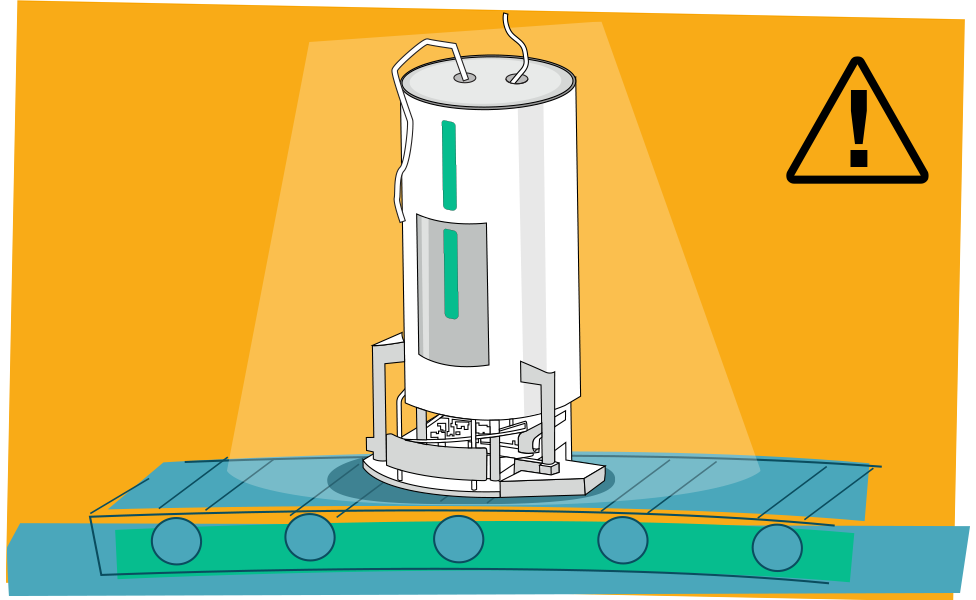
One of the most pressing problems has been the shortage of big, sterile plastic bags used to grow vaccine cells inside large vessels called bioreactors.
They are a little like the bags used in the home-brewing process, says Matthew Downham, sustainable manufacturing lead for the Coalition for Epidemic Preparedness Innovations (CEPI) - a global body aiming to fast-track vaccine production and one of the lead organisations launching the marketplace.
The giant plastic bags, which can hold up to 2,000 litres, are needed in the process of making all the four types of vaccine currently in manufacture.
2. Filters and plastic pipes
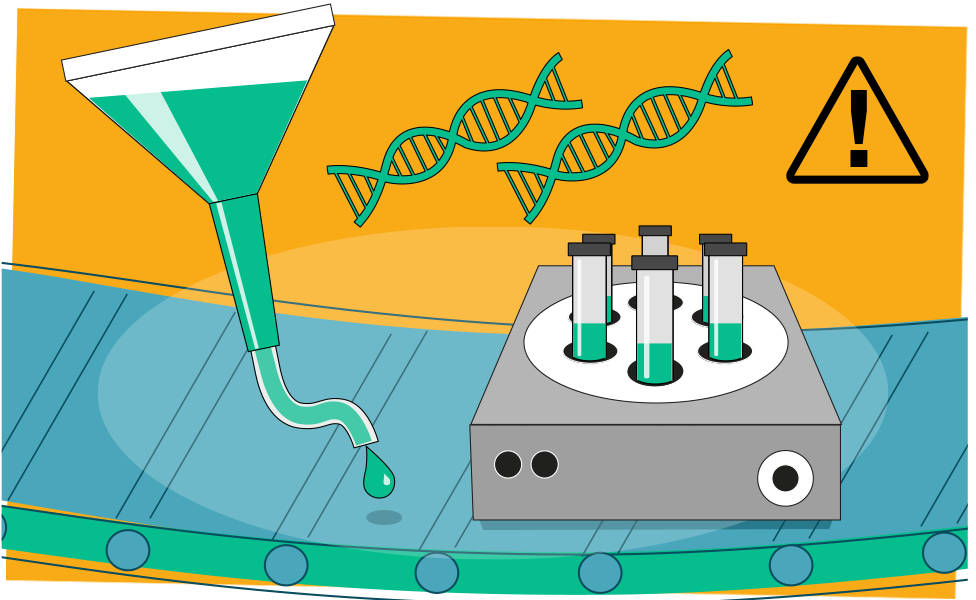
There have also been concerns about the availability of filters and plastic pipes - sometimes referred to as single-use assemblies. Both are, again, required by all four types of jab in production.
The plastic tubes are used in many biological processes, but can only be used once.
3. Raw materials
Essential ingredients for developing cell cultures - used to produce some of the drug substances - have also been in short supply.
There have also been problems with a specialist ingredient called lipid nanoparticles - ultra-tiny particles that are crucial to the pioneering mRNA vaccines produced by BioNTech/Pfizer and Moderna.
Before the pandemic, these nanoparticles - used to house the drug substance for easy delivery into the body - were only produced in small amounts for clinical research, so scaling up has been a big challenge.
4. Trained workers
As vaccine manufacture has ramped up, so has the need for skilled people.
Those involved in the industry say some locations have struggled to find enough trained workers to fill specialist roles.
Mr Downham says companies find it hard to move their people between their own sites, but it is "even more complicated" when transferring staff to another company contracted to do the manufacturing.
To help solve the problem, the pharmaceutical industry wants to see workers able to travel between international sites more easily.
5. Intellectual property?
Whether intellectual property and patent protection are seen as blockers to the current global rollout very much depends on who you ask.
Intellectual property (IP) refers to creations or inventions protected by law through such things as patents, copyrights and trademarks. They aim to ensure the originator is rewarded through profits and that their invention retains quality and integrity.
The US has thrown its support behind a move at the World Trade Organization (WTO) - an intergovernmental body that promotes global commerce - to temporarily lift such patent protection for coronavirus vaccines.
It followed a campaign by India and South Africa and a group of about 60 countries which argue waiving IP protections will allow manufacturing know-how to be passed on more easily.
But vaccine makers say that even if a patented vaccine's IP is released, new companies would not just suddenly be able to make jabs.
They would still need the specialist facilities and expertise and they would be competing for the same limited number of trained staff and materials., external
Albert Bourla, chief executive of Pfizer, argues that a waiver could actually "derail progress" on the global vaccine rollout., external
Dr Liz Breen, a reader in health service operations at the University of Bradford, agrees that releasing IP isn't an instant solution.
"It is only one part of the jigsaw," she says.
How bad is it and what's being done?
Manufacturers are aiming to supply the world with an estimated 11 billion coronavirus vaccine doses by the end of 2021 - a massive increase in capacity, tripling previous annual vaccine output.
But the industry says it can only meet these commitments if the current shortages in materials and components are tackled alongside measures to allow the free flow of workers around the world.
The World Bank has even said the resulting delays could push back the date of worldwide herd immunity, which it had predicted could be reached by March 2022., external
CEPI's Matthew Downham says "there is a tonne of activity going on" to try to relieve the pressures on key components and materials - to get them made and shipped to vaccine makers as fast as possible.
A global manufacturing task force, external - an offshoot of the Covax scheme which aims to ensure vaccines are available everywhere around the world - has been set up to try to tackle the shortages.
And now the Covax Marketplace has been launched - a secure platform that will allow manufacturers and suppliers to buy and sell products in one place, helping to increase the visibility of what's available when.
It will initially focus on six categories of supplies: bioreactor bags, single use assemblies, filters, cell cultures, lipids, glass vials, and stoppers.
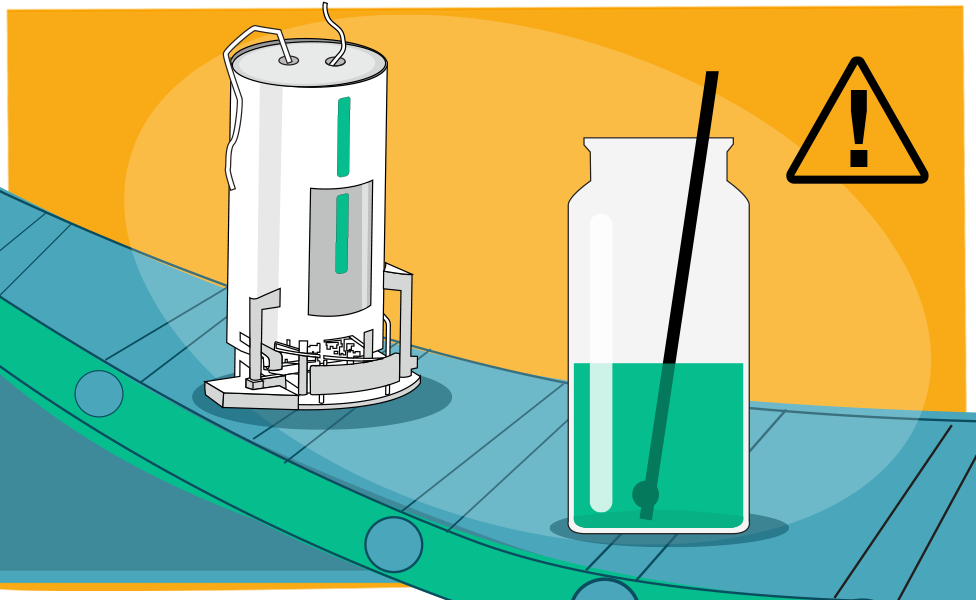
But, Mr Downham says, work also needs to be done to ensure vaccine makers are using their full capacity at all times. For example, if a manufacturer's "fill and finish" services - when vaccines are bottled and packed - are not available, there need to be ways of using other available facilities to ensure manufacturing doesn't slow down or come to a halt.
In the longer term, the manufacturing task force aims to build manufacturing capacity - factories, staff and expertise - across the world, especially in low and middle-income countries.
But with global demand for doses still dwarfing supply, and devastating levels of Covid-19 in places like India and Brazil, the pressure to find quick solutions has never been greater.
The International Federation of Pharmaceutical Manufacturers and Association's Thomas Cueni, at an industry briefing, was uncompromising about what the outcome would be if that demand was not met.
"We would fail the world," he said.
Design and illustrations by Zoe Bartholomew