Children's gender services need transformation - review
- Published

The only NHS gender identity facility for young people in England is based at the Tavistock and Portman NHS Trust
The NHS needs a fundamentally different model of care for children with gender dysphoria to meet their needs, according to a senior doctor.
Dr Hilary Cass, who is leading a major review of the services in England, has published her interim report, external.
She is not yet making recommendations on the use of hormone treatments.
Dr Cass sought to reassure young people who might be anxious while waiting to access NHS support for gender issues, saying services would not be stopped.
"I think that more services are needed for you, closer to where you live," she told them.
The review says that children and young people experiencing gender distress "must receive the same standards of clinical care, assessment and treatment as every other child or young person accessing health services," and stresses that they need to be able to get psychological support.
Long waiting lists
Currently there is a single, specialist clinic offering gender identity services to children and young people in England and Wales - the Gender Identity Development Service (Gids) based at the Tavistock Centre in London.
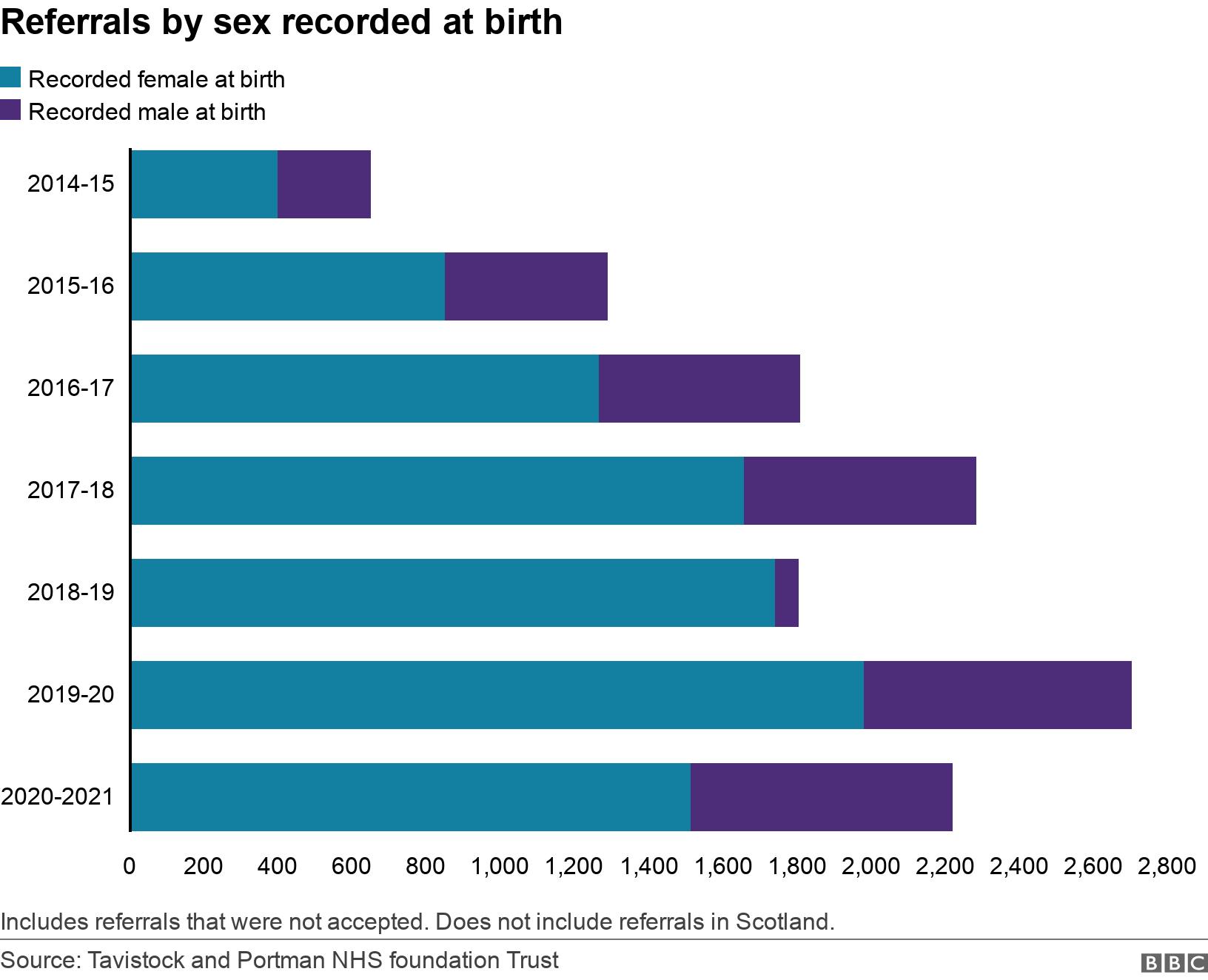
There has been a large increase in referrals to the clinic in recent years, and it has struggled to meet demand.
The clinic was rated as "inadequate" by inspectors who visited in late 2020 after concerns were raised by whistleblowers and reported by BBC Newsnight.
Children and young people are now waiting over two years to be seen without support, and Dr Cass says this delay risks worsening their distress.
The Tavistock and Portman NHS Foundation Trust has said it will work with Dr Cass and NHS England to support her recommendations.

The report notes that many young people using the service have a range of mental health needs, looked-after children are overrepresented, and around a third of those referred to Gids have autism or other neurodiversity.
It describes an issue it calls "diagnostic overshadowing", where a child's healthcare issues which would normally be managed by local doctors can be overlooked after they are identified as having gender-related distress.
Dr Cass supports a plan to move from one specialist clinic to regional hubs, building capacity and reducing waiting times, writing that the current provider model "is not a safe or viable long-term option".
Data collection criticised
The review finds that there "has not been routine and consistent data collection" within the current specialist service, and its approach "has not been subjected to some of the normal quality controls that are typically applied when new or innovative treatments are introduced".
The review team says it is not yet able to advise on the use of physical treatments such as puberty blockers and hormones due to gaps in the evidence base, but is working to develop recommendations.
Puberty blockers - powerful drugs which block the actions of sex hormones and have been used to delay puberty - were the focus of a court case in 2020 in which judges initially ruled that under-16s were unlikely to be able to consent to the treatment. The decision was later overturned by the Court of Appeal.
That case was brought by Keira Bell, who said that staff at the Tavistock should have challenged her more over transitioning.
Dr Cass's report also says that the current system where Gids clinicians make a gender dysphoria diagnosis and then refer on to endocrinologists to prescribe puberty blockers should change, with the prescribing doctors becoming active partners in the decision-making process.
In the short-term, the review group set up to look at cases being referred by Gids for hormone treatment should continue its work, Dr Cass says.

Keira Bell spoke to the BBC's Alison Holt in 2020 about her decision to transition and then detransition back to female:
Keira Bell: 'I should have been challenged on my transition'

Dr Cass says that the largest group of patients now referred to Gids are teenagers, registered female at birth, who first developed gender distress in their early teens, whereas most of the research that has been done is on young people born male who expressed discomfort from an early age.
As this change in the case mix only dates to 2014-5, the review says that it is too early to assess the longer-term outcomes for this cohort "since young people may not reach a settled gender expression until their mid-20s".
In a letter to children and young people at the start of her report, Dr Cass says there is still a lot doctors don't know about the long-term effects of hormone treatments.
"What we will be doing over the next few months is trying to make sense of all the information that is available, as well as seeing if we can plug any of the gaps in the research," she writes.
Elsewhere in Europe, Sweden, external announced new protocols avoiding the use of hormonal treatments for most under-18s last month due to concerns about their risks and the lack of evidence.
The Tavistock and Portman NHS Foundation Trust said in a statement that it welcomed the review's focus on increasing and broadening the care and support available for this group of patients and on developing the evidence base.
"We will work with [Dr Cass] and NHS England to support her recommendations."
- Published1 April 2021

- Published30 March 2021

- Published19 June 2020

- Published12 October 2021
