Are we failing young people with cancer?
- Published

Deborah James paid to have a private examination before bowel cancer was diagnosed
When you think of cancer, a glamorous mum in her mid-30s is not the first image that springs to mind.
But You, Me and the Big C podcaster Dame Deborah James was just 35 when she found out she had bowel cancer. Blood and stool tests had come back normal and her GP had laughed "not once, but three times over the course of six months" at the idea she could possibly have a tumour in her bowels. The diagnosis came only when she paid to have her colon examined privately.
Her experience has raised questions about how good we are at spotting and treating cancer in the under-40s. Simply - are we failing young people with cancer?
There is a big challenge here - cancer is rare when you're a child or a young adult.
Cancers in toddlers do happen, but they are incredibly rare. The risk builds with every birthday, and then rises rapidly after we turn 55.
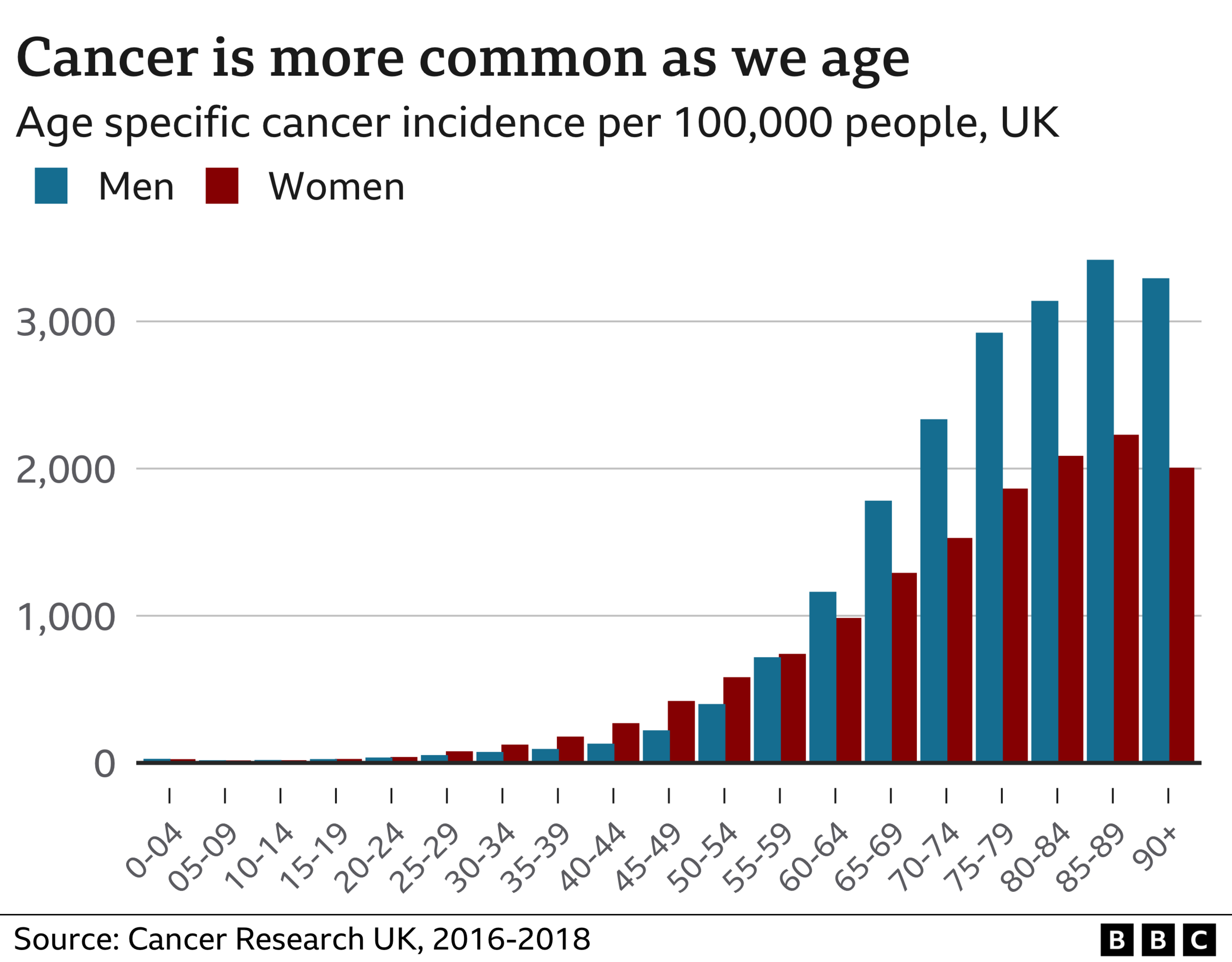
The longer we live, the more time our bodies' cells have to build up the mutations that turn healthy cells cancerous. At the same time our immune system, which also mops up cancerous cells, becomes less effective.
So overall, around 4.3% of cancers diagnosed in the UK are in the under-40s, while those over 75 make up more than a third of all cancer cases.
This poses a challenge for us and the doctors who treat us.
When we are young, we're less likely to attribute any ill health to cancer. Changes to our bowel movements could just be stress, blood in the toilet after we poo could be inflammatory bowel disease or haemorrhoids. Because, for most people, cancer is something that happens to our parents or grandparents.

Charlotte Maden has had surgery for bowel cancer and is waiting to find out if she needs chemotherapy
Charlotte Maden, who's 38 and from Lancashire, was shocked when she was diagnosed with bowel cancer in February.
"I never thought bowel cancer would be an issue for me - I'm young, healthy, not overweight, don't smoke, don't drink much - I'm really quite a fit person," she says.
Charlotte says her friends "think they are invincible, and it will never happen to them".
Your doctor should be alert to major warning signs of cancer, but there is a medical saying: "When you hear hooves, think horses, not zebras". It's a call to look for the most common or likely explanation, and the younger you are, the less likely cancer is to be behind your symptoms. This helps channel the health service's limited resources to those most likely to need them.
But that means some younger people aren't being seen quickly enough, although the problem can affect older people too. Bowel Cancer UK's Never Too Young report, external in 2020 found that four in 10 people surveyed had to visit their GP three or more times before being referred for further tests to see if they had cancer.
"I don't think GPs are a problem," says Genevieve Edwards, chief executive of Bowel Cancer UK. "It [bowel cancer] is rare in younger people... It will usually be something else."
The question is - what if you are the zebra, that relatively rare case who does have cancer at a young age?
Charlotte, who has two children aged five and seven, credits her GP with being "really thorough" when she noticed blood in her stools on a couple of occasions. She was diagnosed following two colonoscopies, and had surgery less than three weeks later.
"If the doctor had said it was probably just piles, I might not have come back. I probably owe her a lot really."
One of the most important things is diagnosing cancer at an early stage. The earlier that tumours are found, the easier they are to treat.
Stage 1 cancers - are small, but haven't spread
Stage 2 cancers - are larger, but still haven't spread
Stage 3 cancers - have now spread to some of the surrounding tissue such as lymph nodes
Stage 4 cancers - have spread to another organ in the body, creating a secondary tumour
Data from Cancer Research UK shows that, on the whole, cancers in younger people are being found earlier than in older people.
Its analysis for the BBC shows that 74% of cancers are diagnosed at either stage one or stage two in people under 40 in England. That figure falls to 46% in people over 40.
That feeds through into survival figures too. If you look at five-year survival figures in nearly all cancers, 15-40-year-olds have the highest survival rates, and the chances fall as you age.
Only 1% of deaths from cancer - around 2,200 a year - are in people under the age of 40.
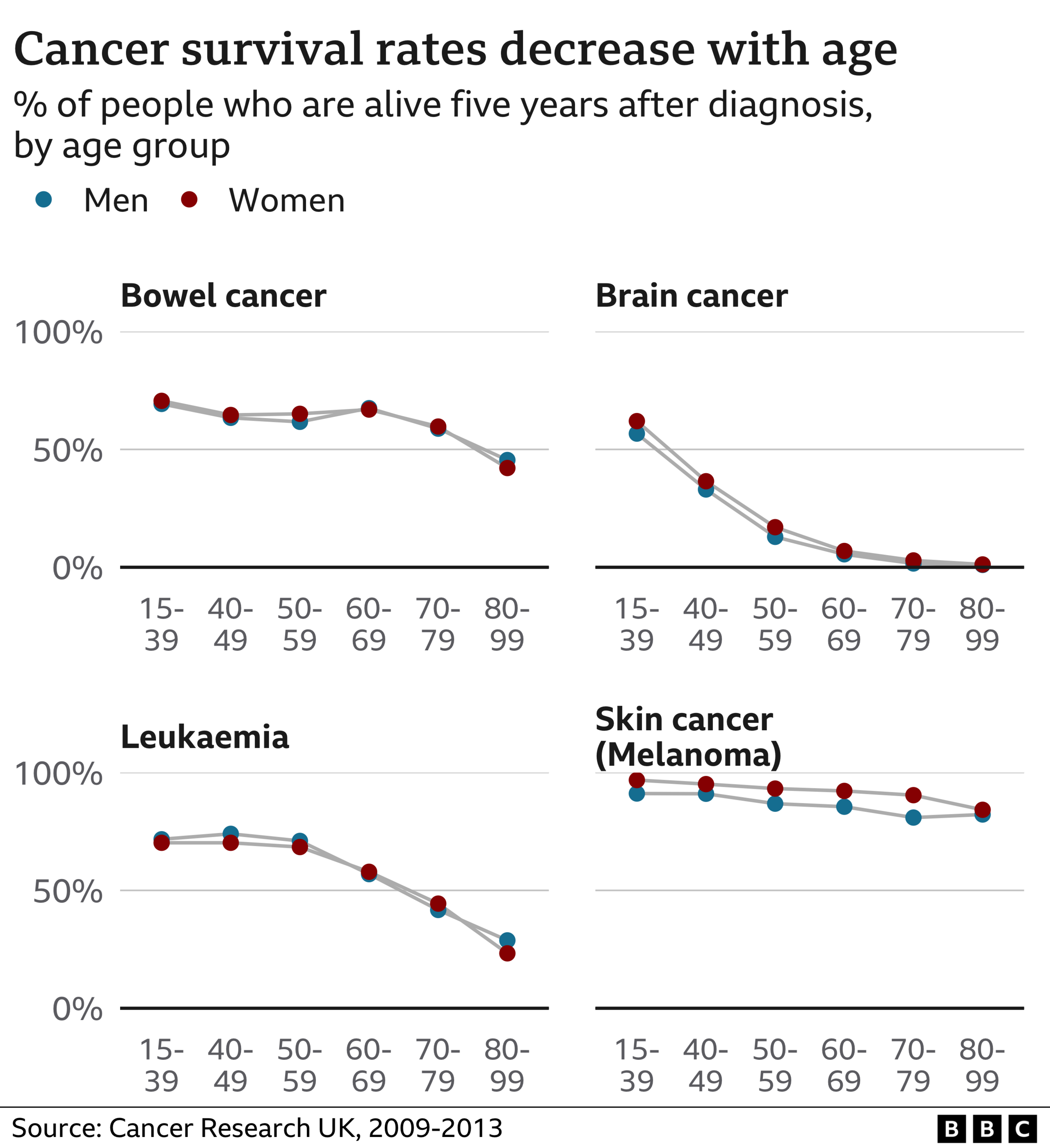
There are notable exceptions to this pattern. Cancer Research UK says survival rates improve in breast and bowel cancer once people reach screening age and seemingly healthy people are checked to see if they have a tumour growing in their body.
For example, bowel cancer is more likely to be found at stage 4 in people who aren't screened (one in four cases in the under 50s) than in those who are eligible for screening (one in five over 50s).
But everyone agrees that you can't screen everybody and it should be concentrated in people who are most likely to benefit. Screening isn't 100% accurate, costs money, and can lead to harm and unnecessary treatment when lots of healthy people are tested.
Screening ages:
Cervical cancer - 25 to 64 years
Breast cancer - 50 to 70 years
Bowel cancer - starts from 50 in Scotland, 60 in England, but is being gradually lowered to 50, 58 in Wales and 60 in Northern Ireland
Are we actually failing everyone?
There is clearly room for improvement in cancer diagnosis and treatment for people, young and old.
The International Cancer Benchmarking Partnership has the difficult challenge of comparing cancer statistics across different countries. It compared seven cancers in seven similar countries - Australia, Canada, Denmark, Ireland, New Zealand, Norway and the UK.
The UK is bottom for survival in five of the cancers, the analysis in the Lancet Oncology showed, external.
Finding cancers is an issue. Before the pandemic, about a fifth of cancers in England were diagnosed only when somebody became so ill they ended up in Accident and Emergency. This could be a bowel cancer becoming so big it actually blocks the intestines, causing a medical emergency. It is no surprise, but cancers found in these circumstances are mostly (around three-quarters) late-stage tumours that are harder to treat, meaning survival is less likely.
The pandemic has made the situation worse, with people not getting checked out and the health service coming under intense strain. GPs in England made more than a quarter of a million urgent cancer referrals in March - the highest figure since records began in October 2009. Cancer charities are worried that queues for tests and procedures which help diagnose cancers, are longer than ever. That creates pressure and delays, and puts people off seeking medical help.
In an ideal world, says Cancer Research UK, people should not wait more than 28 days from being referred by their GP to finding out whether they have cancer - and start treatment within a month of diagnosis.
But to meet these waiting time targets, the charity says GPs need good, timely access to tests: "This will support and encourage [GPs] to refer patients at the earliest opportunity," says chief executive Michelle Mitchell.
And to improve early diagnosis, she wants the government to ensure "the NHS has the workforce and equipment it so desperately needs".
Cancer charity Trekstock says there should be more focus on helping young adults live well during treatment and enjoy life after it's over. This means connecting people, giving them useful information and helping them thrive, says head of programmes Jemima Reynolds.

A tiny capsule containing a camera transmits pictures of patients' insides
What are the solutions?
New tests could help speed up the process of diagnosis.
For bowel cancer, a FIT (Faecal Immunochemical Test) - which looks for hidden blood in poo - can be carried out at home, and used by your doctor to work out if further tests are necessary.
If there is bleeding, you'll be offered a colonoscopy to find out the cause - when a tube with a camera on the end is placed into your back passage to look inside your large bowel.
A new, less invasive alternative is being used by some hospitals in England and Scotland. A colon capsule endoscopy involves a tiny camera the size of a pill being swallowed by the patient. It then takes thousands of pictures as it travels along the gut, allowing doctors to find the cause of symptoms.
The NHS is also running a trial of a new blood test, external which looks for fragments of genetic material from cancerous cells to see if it can help diagnose 50 types of cancer at an earlier stage. But it's not yet known whether the test can help save lives.
Some say greater awareness of cancer symptoms is what's needed - but knowing the symptoms of every cancer is a challenge too.
"General awareness-raising is incredibly hard, and it's very expensive," says Genevieve Edwards, from Bowel Cancer UK. "Just know your body and trust your gut, and if something isn't right, go and see your GP."

Dame Deborah James: The Last Dance
An intimate tribute to Dame Deborah James. Following her death, we hear from friends, colleagues and fellow cancer patients as they celebrate her life and legacy.

Related topics
- Published13 May 2022

- Published11 May 2022

- Published2 May 2022

- Published4 February 2022

- Published29 June 2021
