Monkeypox: How UK hospitals are tackling the outbreak
- Published
The majority of people in the UK who are unlucky enough to catch monkeypox will have a very mild form of the disease and recover quickly at home. A small number, though, may need specialist medical treatment.
That's where a group of NHS hospitals - called the High Consequence Infectious Disease (HCID) network - steps in.
The early symptoms of monkeypox can be hard to diagnose - a fever, headaches or back pain, for example.
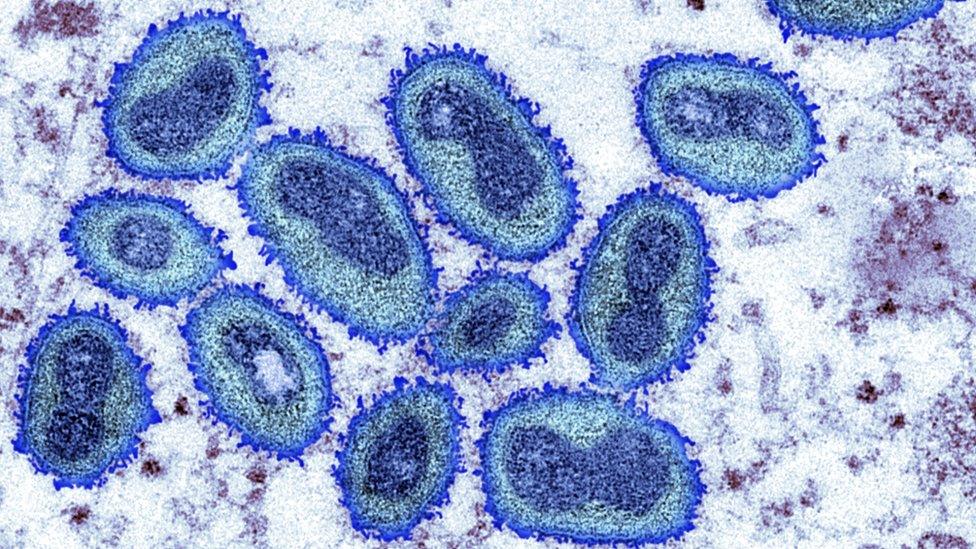
Then a rash starts - often across the face then spreading to the hands, feet and other parts of the body.
It is at that point a patient might go to their local sexual health clinic or GP.
There a swab will be taken and sent to the rare and imported pathogens lab in Porton Down, run by the UK Health Security Agency.
While that is being tested, most patients will be sent home to isolate and recover, and contact tracing teams will be brought in to identify others who might have been exposed.

The rash changes and goes through different stages, and can look like chickenpox or syphilis, before finally forming a scab, which later falls off
It's worth stressing that despite all the media attention, monkeypox is still extremely rare in the UK.
As of Thursday, only 90 people are known to have caught it here in the current outbreak - a fraction of the numbers in parts of West and Central Africa, where the disease is far more prevalent.
A small number may need hospital care.
"Some people do get complications," says Dr Jake Dunning, who diagnosed the first travel-associated case of monkeypox in the UK back in 2018. He is a consultant in infectious diseases at London's Royal Free Hospital, which is treating some of the patients in the latest outbreak.
"They can get secondary infections, they can have more painful lesions that require better control, and also there are some people with risk factors for disease progression. It's those people who we want to keep a close eye on in hospital too."
Knowing the risks
Knowing what those risk factors are in the UK population is difficult, because the data is still so limited.
Based on what doctors know from Cameroon, the Central African Republic and other countries, younger children, pregnant women and people with a severely weakened immune system may be at greater risk of developing a more severe illness.
In parts of Africa, undiagnosed HIV is thought to be a complicating factor, although in the UK, with much greater access to antiretroviral drugs, that is likely to be less of an issue.
The recent strain of monkeypox that has been reported in Europe and the US has had a 3% fatality rate in Nigeria, according to the European Centre for Disease Prevention and Control, external. We don't know how that would convert to countries with much better-funded health systems.

Guy's and St Thomas' in central London is one of five HCID sites in England alongside London's Royal Free, Newcastle's Royal Victoria Infirmary, Sheffield's Royal Hallamshire Hospital, and the Royal Liverpool Hospital
In England, patients developing complications, or in those higher-risk groups, are likely to be sent in a specialist ambulance to one of five dedicated centres: Sheffield, Newcastle, Liverpool or one of two London hospitals.
The HCID network specialises in containing and treating imported illness from Crimean Congo haemorrhagic fever to Ebola, as well as Sars and Mers, the more deadly precursors to the Covid outbreak.
"It's down to having the physical facility and rooms which can safely isolate someone," says Dr Hugh Adler, from the Liverpool School of Tropical Medicine, who treated patients with monkeypox in earlier outbreaks.
"Plus we have the training and the concentration of experts, so there will be teleconferences among the centres most days, just checking how the cases are doing and sharing expertise."
Vaccines and treatments
Those specialist doctors also conduct research, and have easier access to cutting-edge medicines.
In the UK there are currently two main options if a patient has tested positive for monkeypox or thought to have been infected.
The first is to give a vaccine originally designed as an insurance policy just in case a related, but far more deadly disease, should ever start spreading again.
In 1980, smallpox was declared eradicated globally, but the virus still exists in laboratories and there are long-standing contingency plans in case it should somehow get released either deliberately or by accident.
Research shows those same vaccines stockpiled by national governments can also protect well against monkeypox, even if given shortly after someone has already been exposed.
Once symptoms develop though, doctors say the jab is unlikely to have any effect and that is where a new generation of drugs could play a part.

The antiviral tecovirmat, also known as TPOXX, was developed as a treatment in case of a bioterrorism attack
Dr Adler and his colleagues recently published a paper in the Lancet medical journal, external suggesting that the antiviral pill tecovirimat might help reduce illness from the virus.
The data was based on just one patient treated in Liverpool in 2021, but did appear to show she had a shorter hospital stay and developed fewer lesions, or blisters, on her body, compared with other patients.
"If I were to see a severe case, I would be pushing for them to get early antiviral treatment and prioritising antiviral treatment for them," says Dr Adler.
While the experimental use of antivirals has just started in Europe and the US, doctors say the real challenge will be to start clinical trials in parts of Africa where the need is greatest.
Those UK patients admitted in this latest outbreak are likely to spend between between five days and a few weeks in hospital depending on their individual circumstances, doctors have told the BBC.
Those working in specialist hospital units rank the current outbreak as significant and surprising, but say monkeypox is much more straightforward to treat than Ebola, Mers, Lassa fever and other imported diseases that keep them awake at night.
"I never expected to see something of this magnitude, it just seemed so unlikely," says Dr Adler.
"Those of us who were into monkeypox before it was cool, hoped our [research] paper would draw attention to the problem in Western and Central Africa, but we never thought it would be immediately relevant to patients in the UK and across Europe as well."
You can follow Jim Reed on Twitter., external
- Published5 August 2022
- Published10 August 2018
