Hormone replacement therapy and menopause: What you need to know about HRT
- Published
Hormone replacement therapy (HRT) should be offered as the first treatment to ease menopause symptoms such as hot flushes and night sweats, according to the latest advice from health watchdog NICE.
Detailed new analysis suggests HRT does not affect life expectancy - but has benefits and risks that need to be weighed-up by each individual and their medical team.
The updated guidance, external says talking therapies may also help with symptoms.
What is HRT and how can it help women going through the menopause?
As women approach the menopause, their levels of the hormone oestrogen fluctuate and start to drop.
Oestrogen has many roles: it helps regulate menstrual cycles, contributes to bone strength and influences skin temperature.
As levels become unstable, women can experience a range of symptoms, such as hot flushes, night sweats, anxiety and joint pain.


HRT tops up and stabilises falling oestrogen levels.
Those who take it generally don't stay on it forever, just to help with the menopausal transition, and many patients say it made a big difference to their wellbeing.
HRT can also help to prevent bone loss and fractures. For women under 60, it may also offer some protection against heart disease.
You may hear of other potential benefits too - like protecting brain health and improving skin and hair - but so far, the evidence for this is limited.
How do you take HRT and which type is best?
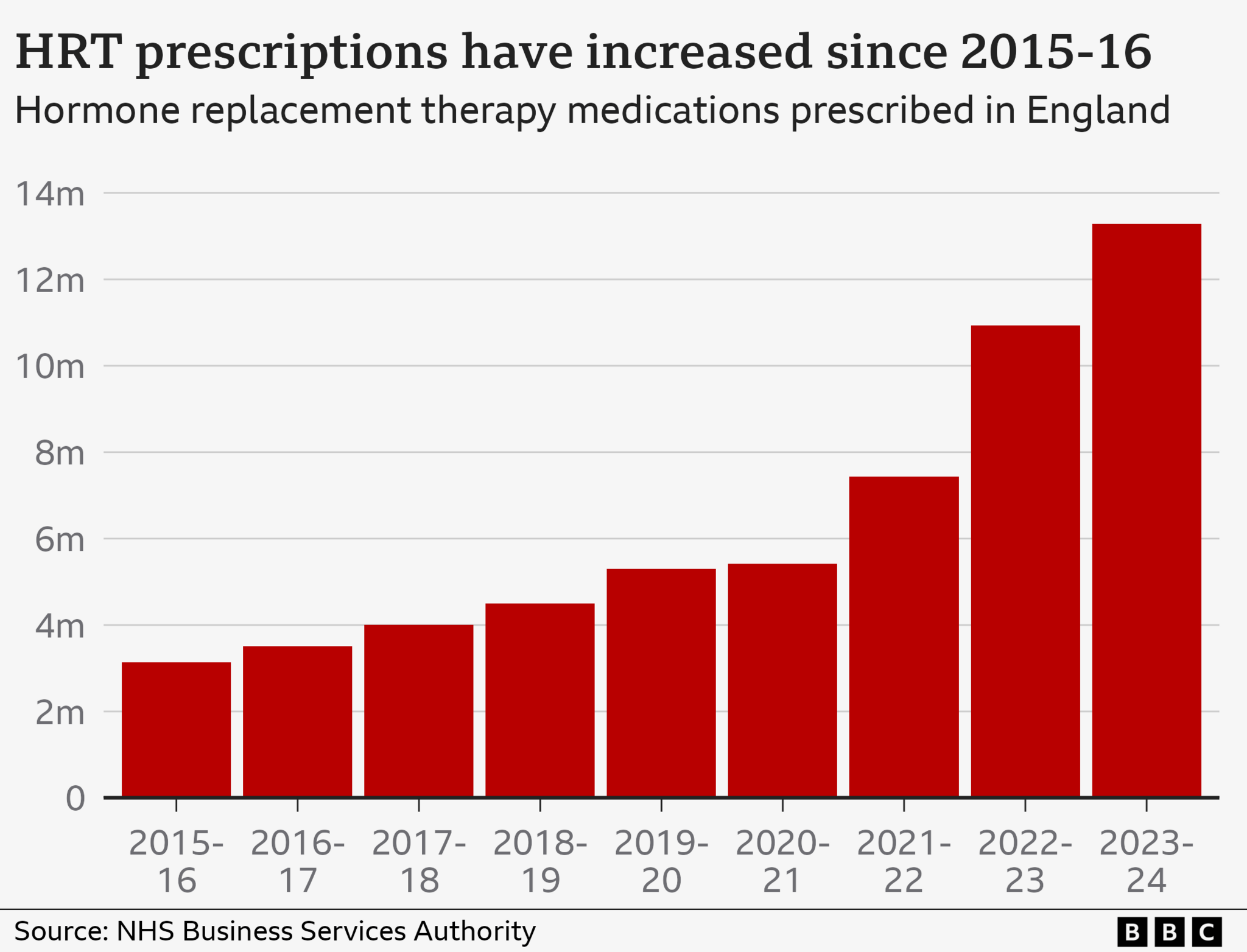
An increasing number of women are using HRT to relieve menopausal symptoms.
The NHS prescribed 13 million HRT items to an estimated 2.6 million patients in England in 2023/24, up from just under 11m items for 2.3m women in 2022/23.
HRT comes in many forms - from pills and patches to gels and rings.
The core ingredient is oestrogen, but combined HRT is commonly available, which also contains a synthetic version of the hormone progesterone.
Adding progesterone helps protect the lining of the womb as oestrogen on its own can sometimes increase the chance of womb cancer.
Most HRT medication works throughout the body, but topical treatments like Gina 10 are used vaginally to relieve symptoms in that area.
This minimises the amount of oestrogen absorbed by other parts of the body, but means those treatments don't relieve other symptoms like hot flushes.
The most effective type of HRT varies from person to person and depends on individual symptoms and lifestyles.
Patients generally start on the lowest possible dose.
How long does HRT take to work?
It can take up to three months to feel the full benefits, and the initial dose and/or type of HRT may need to be tweaked.
Most experts recommend starting treatment when menopausal symptoms first develop.
There is mixed evidence about the effects of starting it over the age of 60, though some older women do experience relief from persistent symptoms.
There is no limit for how long you can take it.
Some experts support taking HRT for many years, but the UK's Medicines and Healthcare products Regulatory Agency recommends using it at the lowest dose and for the shortest amount of time needed.
What are the risks of HRT?
Two studies published in the early 2000s suggested that HRT had more detrimental than beneficial effects.
This got wide publicity and HRT use dropped. Some are still cautious, despite mounting evidence that the treatment can be helpful.
The latest guidance from NICE has detailed tables, external that lay out the potential risks and benefits to help individuals make decisions.
For example, the risk of coronary heart disease was no higher among women aged 45 and over taking combined HRT, compared to those who had never taken it, according to a NICE adviser.
But combined HRT can be associated with a small increase in the risk of breast cancer.
The risk of dementia was also slightly higher if women started taking HRT after the age of 65. In younger patients there was no elevated risk.
There is a small risk of getting a blood clot - although this depends on other factors like smoking, weight and age.
However, the blood clot risk is much lower than if you take the contraceptive pill or are pregnant.
Using HRT skin patches or a gel rather than tablets can also reduce some risks.
Patients are advised to discuss the potential benefits and risks of the different HRT options with their healthcare professional.
What are the side effects of taking HRT?
Side effects of taking HRT can include:
breast tenderness
headaches
nausea
indigestion
stomach pain
vaginal bleeding
Many pass within three months of starting treatment.
It is common to gain weight as people approach the menopause, but there is no evidence HRT is behind this.
Who shouldn't take HRT?
HRT may not be suitable if you have:
had breast, womb or ovarian cancer
untreated high blood pressure
had blood clots
liver disease
are pregnant
What other treatments options are available?
Talking therapy known as CBT (cognitive behavioural therapy) should be offered to women over 40 alongside HRT or, if the patient's individual circumstances call for it, in place of it, according to the latest NICE guidance.
That is a change from controversial draft guidelines, published in late 2023, which suggested that talking therapy could replace HRT as the first treatment option.
Regular exercise may also boost sleep, reduce hot flushes and improve mood.
Eating a healthy diet, cutting down on coffee, alcohol, spicy foods and stopping smoking may also help with hot flushes.
Weight-bearing exercise, such as hiking, brisk walking or playing tennis, also helps keep bones strong.
Other medication such as Tibolone - which works by mimicking the activity of oestrogen and progesterone - or certain anti-depressants may help, although there can be side effects to taking these.
You may hear about bioidentical hormones, which are precise duplicates of human hormones. There are different kinds:
compounded bioidentical hormones, which are not recommended by the NHS because they are not regulated and it is not clear how safe they are
regulated bioidentical hormones, which are authorised as they are seen as safe and effective in treating menopause symptoms
Speak to a doctor or pharmacist if you are considering complementary therapy for menopause. It may not be regulated and the ingredients cannot always be guaranteed.