Dying patient should have been seen in person
- Published

David Nash had an abscess on his brainstem, which was listed as a cause of death
NHS officials ruled a man who died after his ear infection was not picked up in GP telephone consultations should have been seen face to face, a BBC Newsnight investigation has found.
David Nash, 26, had four remote consultations over three weeks during Covid restrictions but was never offered an in-person appointment.
His infection led to a fatal abscess on his brainstem.
The surgery, in Leeds, said it could not comment ahead of an inquest.
Medical documents and recordings of the consultations suggest he should have been given a face-to-face appointment on one of the four consultations he had, according to NHS England.
David first spoke to the practice on 14 October 2020, after finding lumps on his neck.
He sent a photograph but was never examined.
With David worried the lumps might be cancerous, the GP asked a series of questions about his health and reassured him that while she could not rule it out completely, she was not worried about cancer.
She suggested he booked a blood test for two to three weeks' time.
In those three weeks, David would go on to speak to another GP and two advanced nurse practitioners but never face to face or via video call.
BBC Two's Newsnight programme has heard the calls and seen documents relating the case.
23 October: David spoke to a nurse, reporting ear pain and after a five-minute consultation was prescribed ear drops for an outer-ear infection. In fact, he had a middle-ear infection.
28 October: David reported blood in his urine and a fever, which the doctor treated as a urinary-tract infection. This is despite the fact UTIs in young men are "generally uncommon", according to National Institute for Health and Care Excellence (NICE) guidelines, and the doctor himself stating in the call: "You don't seem to have any other signs of a urine infection."
2 November: In the fourth and final call, David said he had debilitating neck pain preventing him sleeping, pain in his sinuses, had had fever for 10 days and was slurring his words. The nurse he spoke to diagnosed a flu-like illness and prescribed pain relief for his neck
"Pretty much every time my heart beats, I'm getting these pains," David told the nurse.
He was actually due to be seen in person at the GP surgery that day, for the blood tests booked some 19 days earlier, when he had presented with neck lumps.
But - fearing he could have coronavirus, despite a negative PCR test - the nurse cancelled the bloods and asked David to retest for Covid.
In its investigation, NHS England found "the overarching benefit [of this decision] was less than the risk with going ahead with blood tests".
'Appalling care'
"What we know now," David's father, Andrew Nash, told Newsnight, "is that a couple of days previously, he more than likely started to develop a brain abscess that was triggered by his ongoing infection in his ear.
"Two and a half hours after that call, David took a selfie of himself to send to a friend."
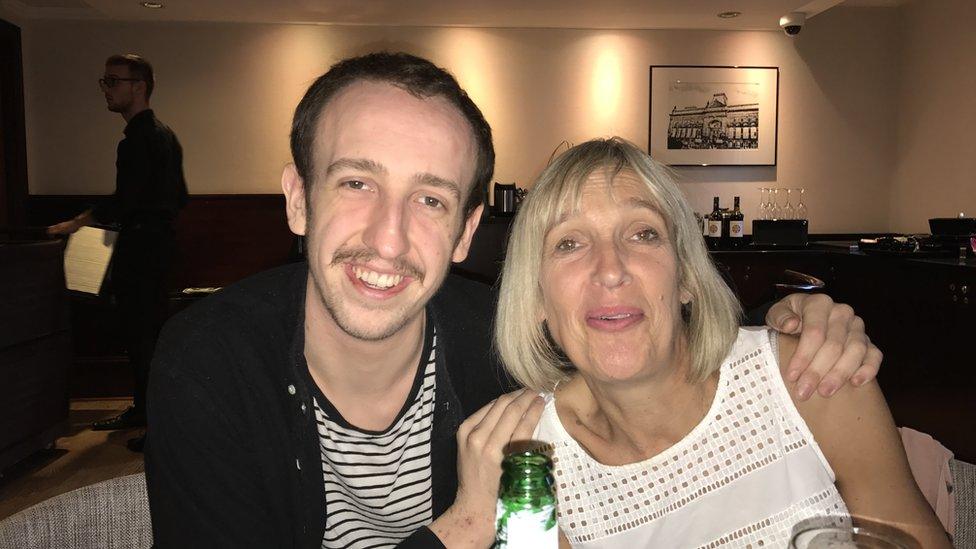
David with his mother, Anne
Newsnight has seen the picture, the last taken of David alive.
"I have no formal medical training other than first aid," Andrew said. "But if I was to identify a picture of someone who was dying..."
After five calls to NHS 111, David was taken to hospital in an ambulance that day but died two days later.
NHS England - in a finding seen by Newsnight - said: "A face-to-face assessment should have been offered or organised to confirm the diagnosis and initiate definitive management."
Andrew added: "He made numerous attempts to access treatment and there were so many opportunities where, had he been seen face-to-face, things would have been different."
Andrew's mother, Anne, said: "It's been appalling care. I think they've completely let David down… at every single point.
"I am absolutely convinced, as David's mum, that if he'd been seen on that last consultation, he would still be with us today."
'Clinical risk'
An inquest into David's death, scheduled for early next year, is expected to also examine what his family say were failures once he had been admitted to hospital.

Andrew Nash said his son had made numerous attempts to access treatment
In documents seen by Newsnight, an independent GP expert who has looked at the case in detail said there were "several points in time where David should have been reviewed face to face".
Dr S L Brown - a GP since 1984 - said he could not determine whether David being seen earlier would have changed the outcome but to prescribe pain relief when he had been so unwell "was a breach of duty".
In a statement, David's surgery said: "We would like to again extend our condolences to Mr Nash's family and our thoughts are with them at this difficult time.
"It would not be appropriate to comment further as the inquest is ongoing."
NHS England, North East and Yorkshire, which investigated David's death, offered its condolences to the family.
"We have investigated the family's complaint regarding their son's treatment within primary care and provided them with a response", it said in a statement.
An NHS England spokesperson said: "The NHS has made it clear that every GP practice must offer face to face as well as telephone and online appointments, and that clinical judgement alongside patient preference must be considered."
In June, the Nuffield Trust published a report that found "the clinical risk from remote consultations is not yet well understood".
"Remote consultations also carry some risks - missed or delayed diagnoses due to loss of information from visual clues, physical examination and 'door-knob' concerns [fresh issues raised by patients towards the end of face-to-face consultations], missed signs of safeguarding risk, lost opportunities for public-health interventions and increased use of investigations and referrals to other services," the report said.
A Department for Health and Social Care spokesperson said: "We are clear that practices should respect patient preferences for in-person appointments where expressed."
Additional reporting by Charlotte Rowles and Emily O'Sullivan.
How have you been affected by the issues raised in this story? Share your experiences by emailing haveyoursay@bbc.co.uk, external.
Please include a contact number if you are willing to speak to a BBC journalist. You can also get in touch in the following ways:
WhatsApp: +44 7756 165803
Tweet: @BBC_HaveYourSay, external
Please read our terms & conditions and privacy policy
If you are reading this page and can't see the form you will need to visit the mobile version of the BBC website to submit your question or comment or you can email us at HaveYourSay@bbc.co.uk, external. Please include your name, age and location with any submission.