NHS care backlog push at serious risk - National Audit Office
- Published
- comments

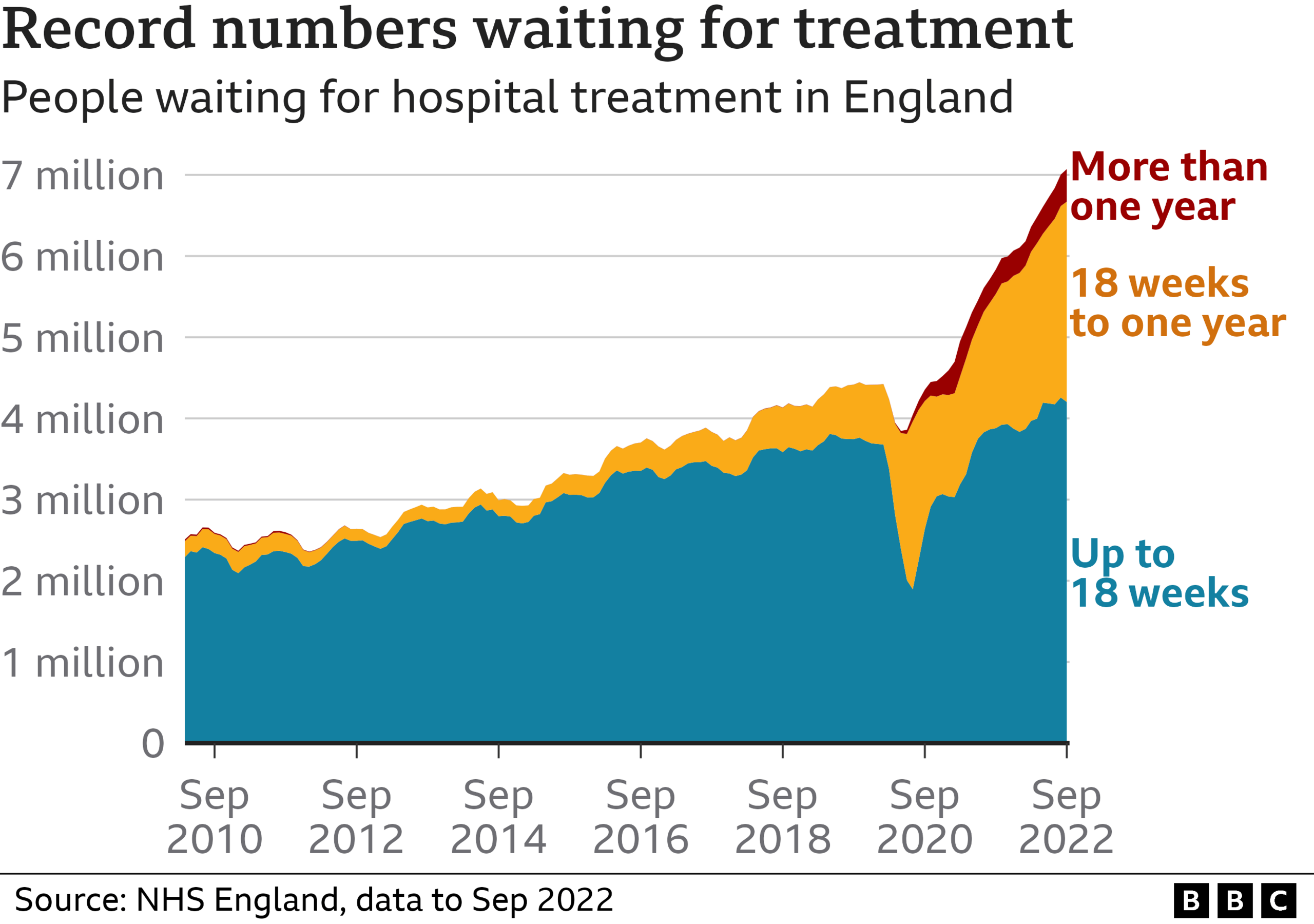
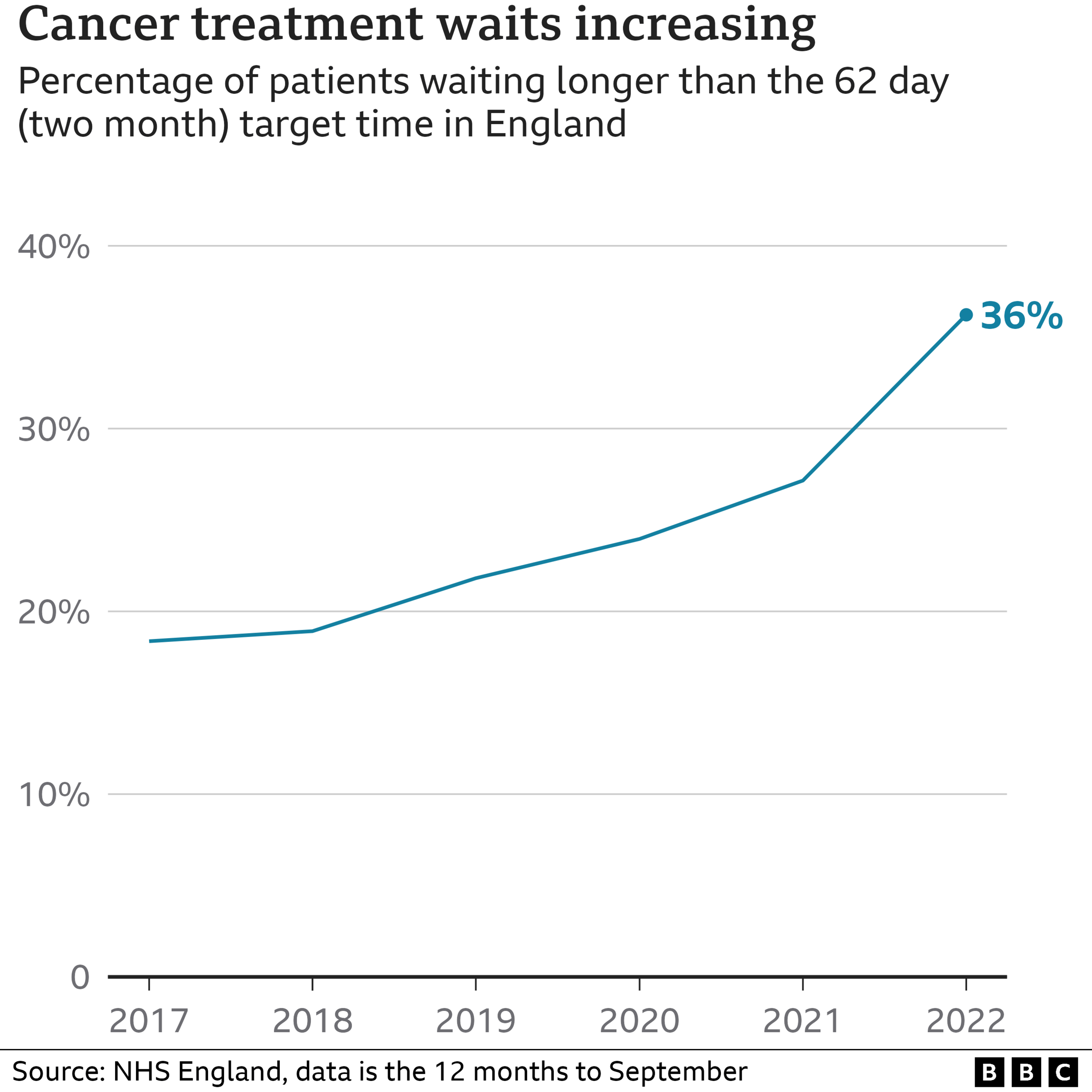
The plan to tackle long waits in hospital treatment and cancer care in England by 2025 is at serious risk, the spending watchdog says.
The National Audit Office report warned inflation and other pressures on the NHS could undermine the push.
These included a lack of staff and hospital beds, which was affecting productivity, the watchdog said.
But NHS bosses said they could overcome the challenges and the health service was on track to hit its targets.
NHS England and the government have set a series of targets over the next three years.
They include:
returning performance on the 62-day target for cancer treatment to pre-pandemic levels by March 2023
ending waits of over a year and a half for planned treatment, such as knee and hip operations, by April 2023
ending waits of over a year for planned treatment by March 2025
The NAO report comes as the chancellor prepares to set out his tax and spending plans in his Autumn Statement on Thursday.
Cuts to public spending are likely but Health Secretary Steve Barclay has strongly hinted the NHS will receive more money.
Its budget was already due to grow by nearly £5bn next year.
But NHS England has warned that still leaves a £7bn shortfall, because of inflationary pressures.
The NAO said inflation had chipped away at how far the money set aside for backlogs would go.
Its report noted the NHS was still doing fewer planned treatments, such as knee and hip replacements, than before the pandemic.
The goal is to increase them by nearly a third.
The creation of a network of community surgical and diagnostic hubs to test and treat more patients had had less impact than expected, it said, due to:
staff shortages - one in 10 posts is vacant
a reluctance among existing staff to work overtime
Continued high rates of sickness were also a problem.
A lack of support in the community meant most patients ready to be discharged could not be, limiting the number of treatments possible.
The number of fully qualified GPs was falling and there was limited evidence the plan for them to provide support and advice in the community rather than referring patients on to specialists in hospital would work.
NAO head Gareth Davies said the NHS needed more support and to be challenged in areas where it was making insufficient progress.
"There are significant risks to the delivery of the plan to reduce long waits for elective and cancer care services by 2025," he added.
A NHS England spokesman said the health service was facing challenges but remained "on track" to deliver on its goals.
Related topics
- Published9 August 2022

- Published10 August 2022

- Published22 July 2022
