'Major moment in MS research' as new Octopus trial starts
- Published

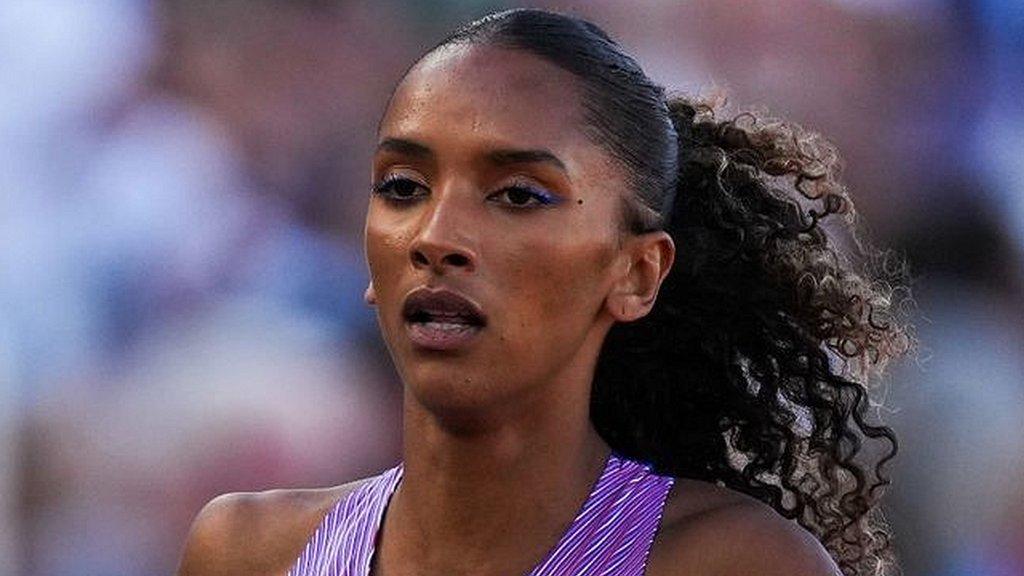
Ailsa was diagnosed with multiple sclerosis when she was 22 years old
"I was playing a game of ultimate frisbee and got fuzzy vision in one eye - a bit like looking through a steamed-up windscreen."
Ailsa Guidi was 22 at the time, studying at University of Manchester.
"The doctor said it was optic neuritis, so I had steroid treatment, and the blurring went away. So I got on with being a student."
Two years later, in 1999, her vision went fuzzy again. This time, her GP was concerned that it might indicate something more serious.
On a Friday evening, Ailsa went alone for her first MRI brain scan with the neurologist who would give her a life-changing diagnosis.
"He told me: 'you've got very mild multiple sclerosis'. At the time I knew some people who had MS and needed to use a wheelchair. My eyes filled up with tears and the neurologist asked me 'why are you crying? I've just told you it's very mild'," Ailsa remembers.
"But I was 24, all my friends were meeting up at the pub that evening, and so for me, it was a really big thing to take in. Even if having milder MS was good, as the neurologist saw it, for me being diagnosed with MS was not."
Ailsa began treatment, and tried not to let the diagnosis change her life too much.
"At the time, I found it quite hard to talk to friends about it because they were either so worried about me that I ended up telling them I was totally fine, or they just didn't know very much about MS," Ailsa recalls.
She saw in the millennium in Barcelona with her boyfriend Robert, who was studying at the same university. Later they married, and in 2005 had their first child.

Ailsa went on to marry and have three children, and is now taking part in a trial of existing drugs to treat MS
MS is a neurodegenerative disease, in which the immune system mistakenly attacks the fatty myelin sheath that protects the nerves in a similar way to insulation around electric wires. As that protection is gnawed away, the nerves can eventually stop being able to send the signals that help us to walk, talk, think clearly or use our hands normally.
'A major moment in MS research'
Ailsa, now 47, is taking part in a groundbreaking new trial, which is looking into whether existing drugs can be repurposed to help slow MS progression.
The way it is designed means several drugs can be tried at the same time, and more can be added or dropped as results emerge.
The Octopus trial - so-called because it is a multi-arm, multi-stage trial - is being run by Prof Jeremy Chataway, from the National Hospital for Neurology and Neurosurgery UCLH in London, with £13m in funding from the UK's MS Society.
A similar trial design has been used to test drugs for prostate cancer and Covid.
Existing trial patients who prove to be on ineffective drugs can swap to a new arm, and are allowed to continue any other MS disease-modifying drugs they may already be taking.
The first two trial medications are high-dose metformin - a diabetes drug that may help regenerate myelin - and a version of high-dose alpha-lipoic acid, which is a food supplement that acts as an anti-oxidant. It has already been approved in Germany for treating neuropathy - weakness, pain, numbness or tingling in damaged nerves.
The trial team spent several years whittling down 100 potential drugs, and will add more as other strong contenders emerge.
"We are at the start of a long journey," says Prof Chataway. "There are now many treatments for relapsing-remitting MS, but far less available for progressive MS. This trial structure is like a machine for testing drugs for progressive MS. We hope to make it an everlasting machine - at least until we have achieved what we want in controlling and ultimately reversing progression in this difficult stage of MS."
He thinks MS patients should eventually be able to take disease-modifying drugs to deal with the inflammatory component of MS and add on any remyelinating drugs that prove to help repair or even stop nerve damage.
"This is a major moment in MS research," Prof Chataway believes. "Octopus has the potential to change the clinical trials landscape around the world, and we won't stop until we have the treatments that transform the lives of everyone with MS."
The first 375 patients are already being recruited for stage one of the trial, with stage two due to bring the total up to about 1,000.
This month, Ailsa became one of the first people to be accepted on to the trial, which is aiming to recruit at another 30 centres around the UK as they are approved.
After a brain scan, blood tests and a thorough neurological examination, she has now received her first dose of trial medication.
Ailsa knows that she may be on the placebo arm getting no real treatment, but she hopes the Octopus trial will help doctors find ways of slowing or halting MS progression, and perhaps even repair some of the damage.
"I've got difficulties walking but I can live with that. I just don't want to get any worse."
'Biggest impact is what MS takes away from you'
Ailsa took medical retirement at 33 when it became clear that she could not manage her MS fatigue while working and taking care of their three children while Robert was working full-time.
Robert, also 47, says MS has had a more noticeable impact on them as a family as the illness has progressed.
"At the beginning, things were fairly normal. But now we have to plan a bit more, and take the right equipment. It limits the scope of what you can do, so sport or dancing aren't options any more. The biggest impact is the things that MS takes away from you," he says.
"Ailsa and I are a very close partnership and I think we're both positive people. Everyone has their own struggles in life, so you've just got to get on with it and enjoy life as much as you can."
Why the immune system goes rogue in this way for about three million people worldwide has long been debated. A Harvard University study in 2022 showed compelling evidence that the Epstein-Barr virus that causes glandular fever triggers the process. More research is taking place in the hope that one day, MS can be prevented.
As Ailsa's symptoms progressed, she went from using a single stick or crutch for balance, to a walker, and now a wheelchair, trike or mobility scooter for longer distances, such as when walking the family labrador with Rob or the children.
"I think it's important to be really open with the children, so they understand MS and the impact in their own way," she says.
"And obviously the impact changes. When the children were small, they understood that it may mean you can't join in the mums' race at school, or you might have to do it on your trike. And as the children grow older, they might have to help push my wheelchair when I take them shopping."
In February 2022, Ailsa was given the unwelcome news that she had gone from having relapsing-remitting MS, in which symptoms often improve after a relapse, to having secondary progressive MS, when symptoms no longer clear up after years of cumulative nerve damage.
About 130,000 people in the UK live with MS, and of those, tens of thousands - like Ailsa and me - live with a progressive form of the disease.
Under the current National Institute for Health and Care Excellence guidelines, only two drugs - Siponimod and Extavia - are approved for secondary progressive MS, and not everyone will qualify for them.
Ailsa discovered this spring that she does not meet the criteria for Siponimod.
"That was a new thing to deal with, because facing progressive MS feels quite different when you run out of disease-modifying drug options. It means that your life has changed in quite significant ways."
'Ability to revolutionise treatment'
Dr Emma Gray, assistant director of research at the MS Society, says the Octopus trial should significantly speed up how quickly treatments can be tested.
"We wanted the trial to be as inclusive as we could, including people up to the age of 70 and those who can't walk, because we often hear from people with more advanced MS that they can't access other studies. My hope is that with Octopus, we have created a world-first platform trial that has the ability to revolutionise the treatment of people with progressive forms of MS - and that this really does change the landscape for MS for good."
For people like Ailsa - and me - with more advanced MS, this trial does offer hope.
I am currently on the same hospital's MS-STAT2 simvastatin trial, testing whether a high-dose statin can limit brain atrophy in MS. That trial is now drawing to a close.
If such repurposed drugs are shown to be effective, that could help thousands of people with progressive MS who otherwise risk being told there is nothing more their doctor can do.
Related topics
- Published9 December 2022

- Attribution
- Published2 October 2022