Martha's rule: Call for right to second opinion after tragic teen death
- Published
Watch: Martha Mills' mother, Merope, shares her struggle with her loss
The parents of a teenager who died in hospital two years ago are calling for patients to be given the right to an urgent second opinion, if they feel their concerns are not being taken seriously by medical staff.
Martha Mills, who would have been 16 on Monday, died after failures in treating her sepsis at King's College Hospital.
An inquest, external said she could have survived had her care been better.
Martha's mother, Merope, has been speaking exclusively to the BBC.
She told BBC Radio 4's Today programme that her family were not listened to by senior doctors on several occasions and were "not given the full picture" about Martha's deteriorating condition - leaving them unable to speak up for better treatment.
She wants hospitals around the country to bring in "Martha's rule", which would give parents, carers and patients the right to call for an urgent second clinical opinion from other experts at the same hospital if they have concerns about their current care.
The hospital that looked after Martha has admitted mistakes were made, external and the trust said in a statement that it "remains deeply sorry that we failed Martha when she needed us most".
An NHS spokesperson said: "All patients and families are able to seek a second opinion if they have concerns about their care and, as professional guidance for doctors in England sets out, it is essential that any patient's wishes to seek a second opinion are respected."
Martha's story
The happy 13-year-old had been enjoying her summer holidays - "her days filled with books and memorising song lyrics", Merope, an editor at the Guardian, recalls., external
But while Martha was on a family holiday in Wales, cycling on a flat and "family friendly" path, she slipped on some sand.
She fell on to the handle bars of her bike, with her abdomen taking the full brunt of the tumble.
Merope told the BBC: "At first, we thought she was just winded because there wasn't any blood or [a] cut.
"It didn't look like anything serious. But it turns out that the force of the fall pushed her pancreas against her spine, causing a laceration.
"It was a difficult, tricky injury, but it did not have to be a fatal one," Merope says.
Martha was transferred to the children's liver team at King's College Hospital NHS Foundation Trust - one of the few teams in the country that specialises in dealing with young people with pancreatic trauma.
After a few weeks on the ward, she developed an infection that would not go away and her condition worsened drastically.
Martha had developed signs of sepsis - when the body's response to an infection is overwhelming and ends up injuring its own tissues and organs.
A subsequent inquest and medical reviews into her death revealed this was not managed properly.
One of the major failings was Martha not being transferred to intensive care quickly enough to support her organs as they became overwhelmed.
The coroner said;, external "If she had been referred promptly and had been appropriately treated, the likelihood is that she would have survived her injuries."
Reviews suggest there had been several missed opportunities to act.
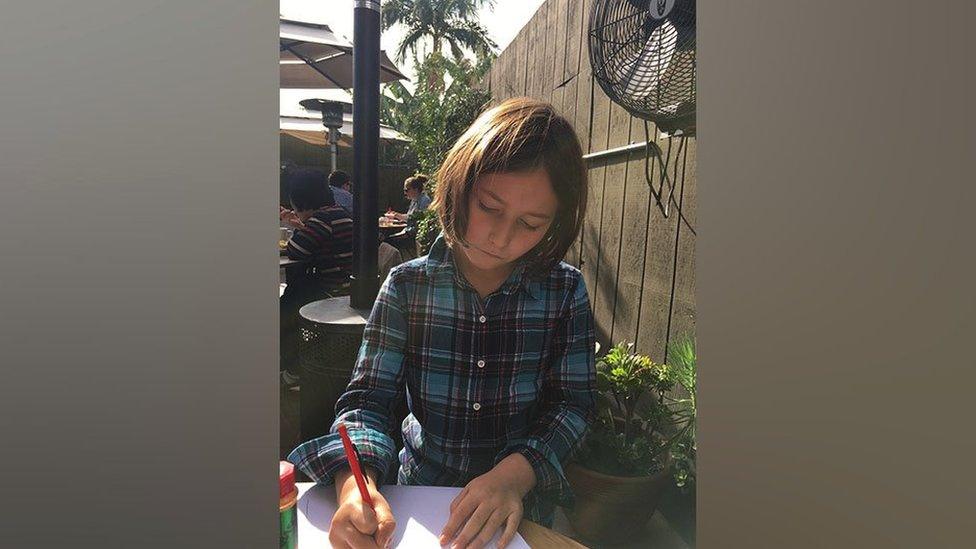
Martha wondered about becoming an author, an engineer or a film director
Merope said as her daughter's condition started to worsen, the family's concerns were not taken seriously.
"She started bleeding out of the tube in her arm... and one in her abdomen as well.
"It was a lot of blood as well, you know, soaking her sheets, and at night, we had to keep changing them.
"The doctors just told us it was a normal side effect of the infection, that her clotting abilities were slightly off."
But Merope says some experts have advised her that this is the point her daughter should have been moved to intensive care - as the bleeding was probably a sign of very disordered clotting and severe sepsis taking hold.
The bleeding did stop, but the infection did not go away and Merope was concerned that the August bank holiday weekend was approaching, when it might be more difficult to get hold of certain staff.
"We started putting two and two together and started using the word sepsis ourselves.
"I said to the consultant, 'I'm worried it's going to be a bank holiday weekend, and she's going to go into septic shock, and none of you will be here'."
But she was "reassured again".
"And so we weren't listened to and Martha herself was ignored."
Martha had further worrying signs of sepsis including a rash that that was mistaken for an allergic reaction, but it was after Martha had a fit in her mother's arms that she was finally transferred to intensive care.
Merope said: "The thing that I find most unforgivable, is that they left her so long, she knew she was going to die.
"She lay in bed and she said to me it feels like it's unfixable."
By this point "it was too late for them to do anything and a day later, she was dead".
The day before her death, Martha was moved to London's Great Ormond Street Hospital as an emergency transfer.
Merope wants to speak out to avoid others going through the same agony.
"Even if you were to give the doctors the benefit of the doubt and say they were trying not to worry us, the result is that they did not give us any agency in demanding the correct treatment for our daughter - and that control - that overconfidence in yourself and your decision-making - is absolutely fine if the system works perfectly, but the system is so far from perfect."
In this video from 2022, Merope asks questions about doctors' attitudes after Martha's death
Merope has helped the think tank Demos write a report, external which is calling on NHS England to urgently put in place Martha's rule.
This would "effectively formalise the idea of asking for a second opinion, from a different team outside the team currently looking after you if you feel you are not being listened to", she said.
She added that asking for a second opinion when there is a deterioration "shouldn't be a problem and it shouldn't involve confrontation".
It might be that a patient or family could escalate to another team over the phone to get an urgent critical care review.
Some similar systems exist already around the world, including one at the UK's Royal Berkshire Hospital.
Here people who are worried a patient is deteriorating, but that the healthcare team is not recognising their concerns, can ring a critical care hotline for immediate help.
In Australia, hospitals in Queensland have a process called Ryan's rule, which came into effect after the tragic death of a boy called Ryan who also had a poorly managed serious infection.
Merope acknowledges that some medics would have concerns that the system could be overrun, but reviews have shown this not to be the case.
When the Royal Berkshire NHS Trust first tried it, there were just 37 calls to the system in the first year - some resulting in life-saving interventions.
She said: "I genuinely believe that good doctors should welcome good input from patients or family members - who are the other experts in the room - and they should certainly welcome the input and second opinion of another doctor."
King's College Hospital said it had put several measures in place since Martha's death, including sepsis training for all clinical staff looking after children.
New hospital guidelines recommend the "escalation of a child's care in those cases where we are unable to provide sufficient reassurance to parents".
And the trust has introduced a specially trained team to review seriously unwell children on wards.
BBC Radio 4's Mishal Husain asked Merope how she is coping now.
She said: "In all honesty, her sister is what gets me through the day.
"Martha would be 16 and I think about her all the time, every day.
"I think about what she'd been doing and how much fun she would be having and how much fun she has already missed.
"I hope in having these conversations we can stop other people going through this horror."
Sign up for our morning newsletter and get BBC News in your inbox.

Related topics
- Published6 October 2022
