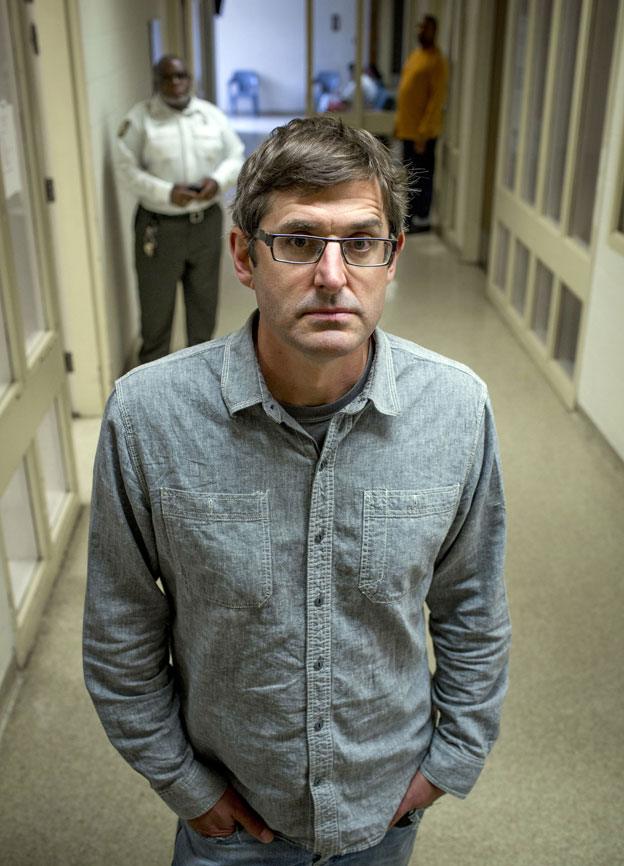
Louis Theroux: The people who are not guilty by reason of insanity
- Published

Every year in the US, courts find people not guilty by reason of insanity. Treating and evaluating them is a painstaking business, writes Louis Theroux.
On my first day at Ohio's Summit Behavioral Healthcare Hospital I met Jonathan. Thirty-nine years old, at one time he'd been an engineering student. But for the past seven years he'd been confined to a mental institution.
He showed me his room - it was bare but not uncomfortable, decorated and furnished in the style of a modern hospital. He had fitness magazines by the bed and a small selection of books.
Then he told me his story - how he had killed his father, stabbing him to death seven years earlier while in the grip of mental illness, before being found NGRI, not guilty by reason of insanity, and sent to Summit.
My idea had been to get to know some of the patients at a top American forensic facility. I wanted to meet men and women who have done some of the worst crimes imaginable - not through choice but under the influence of mental illness.
I was curious about treatment and also about the fraught decision-making process of releasing a patient knowing there is a small chance that he or she may relapse and commit another crime.
After months of approaching institutions around America we had gained access to Ohio's state psychiatric hospitals. In many respects it is a model system - well-funded and focused on rehabilitation.
It is important to note that most of the patients in Ohio's mental health facilities have never committed crimes. They are institutionalised because they have lost touch with reality and are having problems functioning unaided in the community. Indeed, in general, people with mental illness are much more likely to be the victims of a crime than the perpetrators.
However, a small proportion have committed crimes, sometimes of the most gruesome kind.
It was their stories that I was interested in.
Meeting forensic patients for the first time could occasionally be an unnerving experience.
They often came across as mild and gentle people, but the details of the crimes were harrowing in the extreme.
In the four weeks I spent at the hospital, I spent time with - to mention just three - a man who killed his infant daughter, another who stabbed a stranger to death on the streets, and a third who sexually assaulted his mother (he was under the delusion that she would enjoy it, he told me). In each case, the men were polite and obliging and still struggling to understand how they'd come to commit their crimes.

Summit Behavioral Healthcare Hospital
In Jonathan's case, his father had been a much-loved history professor in a small college town in the south-eastern corner of Ohio.
Jonathan had been the elder of two boys. His upbringing had been unremarkable, though he told me his family had been a little emotionally reserved.
Jonathan had been a good student. But at some point in his twenties, during his postgraduate studies, he'd begun suffering the symptoms of schizophrenia and become convinced, with no evidence, that his father had sexually molested him as a child.
On the day of the offence, he stopped by his father's house, took a knife from the kitchen and used it to kill his father. Newspaper reports described stab wounds to Jonathan's father's eyes.
Treatment at the hospital involves a combination of classes and inter-personal therapies, combined with a regimen of psychoactive medication. Doctors and therapists like to say that "medication is only half of treatment but it's the first half".
The non-pharmaceutical therapies range from the traditional chats about thoughts and feelings to lessons in dressing for a job interview, cookery classes, and also support groups for those with drug and alcohol problems.
The medications aren't always effective - some patients experience dramatic improvements, others remain in psychosis long-term, unresponsive to the doctors' best efforts to bring them back into reality.

I had several conversations with patients in psychosis and never quite got used to it.
One thought he was the real President Obama, a second was under the impression that he was doing deep-cover work for a secret government agency.
On the same unit as Jonathan, I played a game of cards with a patient named Judith. She'd been locked up after being accused of stabbing a woman on the bus with a pair of scissors.
The conversation proceeded very pleasantly - we talked about the BBC and her bridge group, and then something strange happened. She mentioned that other patients on the unit would, from across the room, chew food that was in her mouth.
In my early days at the hospital I made the mistake of directly challenging some of the delusions, before realising it was a futile effort.
With time, I found it more productive re-directing the conversations away to more solid ground.
Then there were the grey areas.
William prepares to leave hospital
A patient named Brian had beaten his mother to death with a baseball bat, believing her to be possessed by the Devil. Brian was a Pentecostal Christian. He'd been doing well in treatment, but one of his obstacles was that he still believed his mother had been possessed - only now, he conceded that the killing was a pointless act, given that the Devil can't be killed.
Brian presented a dilemma for the hospital. They viewed some of his beliefs as a kind of psychosis - and yet they were also part of a worldview shared by millions of mentally healthy people.
Jonathan had been one of the more fortunate ones inasmuch as his illness responded well to medication.
Having initially been convinced that he'd been justified in killing his father, he gradually came to realise that his father had never abused him and that the killing had been a senseless act of madness.
"It was challenging," he said. "That meant that I had done something very wrong. It's hard to accept that one has had false beliefs."
In the years since, Jonathan had been making steady progress through the hospital's five "movement levels" that dictate the patients' level of treatment.
Each patient works closely with a treatment team - a conclave of psychiatrist, psychologist, social worker, and other clinicians, which tracks their progress and sets clinical goals each month.
Not surprisingly, the clinicians on the treatment teams develop a rapport with the patients in their care. In a very human way, they root for their patients' recovery.
At the same time, they are under pressure to make the right call on whether to increase a patient's movement level. Simply put, how do you know when someone who has done something terrible but now appears well is safe for release?
If a patient's release goes awry, the consequences can reverberate for years.
At a mental hospital in Columbus I met Eric. He was pushing a trolley of "comfort items" for delivery to other patients: cuddly toys and toiletries.
An older man, deep-voiced, he exuded friendliness and gentleness.
He'd first been detained in 1985, having been found NGRI for the robbery of a beauty parlour. But after four years in the hospital, Eric had gone out on a weekend pass, stopped taking his medication, and shot and killed two strangers in a bar.
Twenty-six years later, he remained at the hospital, stalled at Level 2. He was confined to the corridors and units, with the possibility of never being released - his story a constant reminder to the hospital of how badly wrong a release can go.
On one of my last visits to the hospital, I sat in with Jonathan as he went before a Forensic Review Team - the panel of clinicians that assesses patients for an increased movement level.
He was to be considered for Level 5, which would permit him short unsupervised visits into the community.
If it went well, the man who'd stabbed his father to death would be venturing out into the normal world on his own, sharing streets and parks and cafes with regular members of the public.
Afterwards the two clinicians pronounced that he'd passed his review with flying colours.
It was oddly touching seeing Jonathan sharing the good news with his Lithuanian-born psychiatrist, Dr Rukseniene.
I told her she seemed pleased.
"Of course," she said, blushing. "He is our project."
By Reason of Insanity: Part 1 will be broadcast on 22 March on BBC Two at 21:00 GMT. You can catch up via the BBC iPlayer
Subscribe to the BBC News Magazine's email newsletter to get articles sent to your inbox.