The woman who wanted her pacemaker turned off
- Published
Pacemakers have been used to treat a variety of heart conditions for more than 50 years
A case thought to be the first of its kind in the UK has highlighted a complicated ethical and legal dilemma - is it right to turn off someone's pacemaker, if that's what they want?
Nina Adamowicz was asking for a procedure that would lead to her certain death.
Heart disease runs in her family, and she had had her first pacemaker fitted in 1996. For 10 years, it was great. Then she had a mild heart attack and her health deteriorated. She said she had excellent care, but by late 2014, her heart was working at less than 10% capacity. She was unlikely to have long to live.
"I feel like I am in line for execution," she told the BBC in January 2015.
Adamowicz, then 71, described how she would lose consciousness, often at night, and would hear the click of her pacemaker snapping into action when she came to. She said she was "lucky", and "forever grateful" for her life, but that she was also prepared to die.
"I feel that [there is] life, and death is other side of the same coin," she said.
"I'd like to know what is there.
"It's not about 'I want to die', I'm dying."
So she asked for the pacemaker to be turned off.
The request put her doctor in a bind. The case was referred to her local hospital trust's ethics committee, which was concerned that the doctor would be open to prosecution if he performed the procedure and indicated her request was unlikely to be agreed.

Find out more
Nina Adamowicz spoke to Radio 4's iPM programme
You can also listen to the original interview broadcast in January 2015

Adamowicz's case is the first known instance of such a request in the UK, but the practice of turning off pacemakers is more common in the US. In a career spanning more than 30 years, Dr Westby Fisher, a cardiac specialist at North Shore University Health System in Chicago, has been asked to deactivate a pacemaker or other heart device about a dozen times. He compares the procedure to withdrawing a feeding tube or turning off a ventilator.
"To allow the patient the opportunity to make their own decision is incredibly important," he says.
Fisher described one case of a patient who had a pacemaker for years before a fall down a staircase led to severe bleeding in his brain.
"The family did not want to prolong the inevitable dying process and asked me to turn off his pacemaker," he says.
"I told them what to expect, I told them how the pacemaker was working at the time and that there was a chance that when we turned the device off his heart could completely stop, or he may have a very slowed rhythm, and they would have some additional time to spend with him before he completely died.
"I spoke with the patient's wife and she was very forthright and determined that this is what she desired for her husband and that this would have been what he would have wanted."
Fisher allowed the wife to take the final step by touching a computer screen to turn off the radio-controlled pacemaker. The patient died the following day.

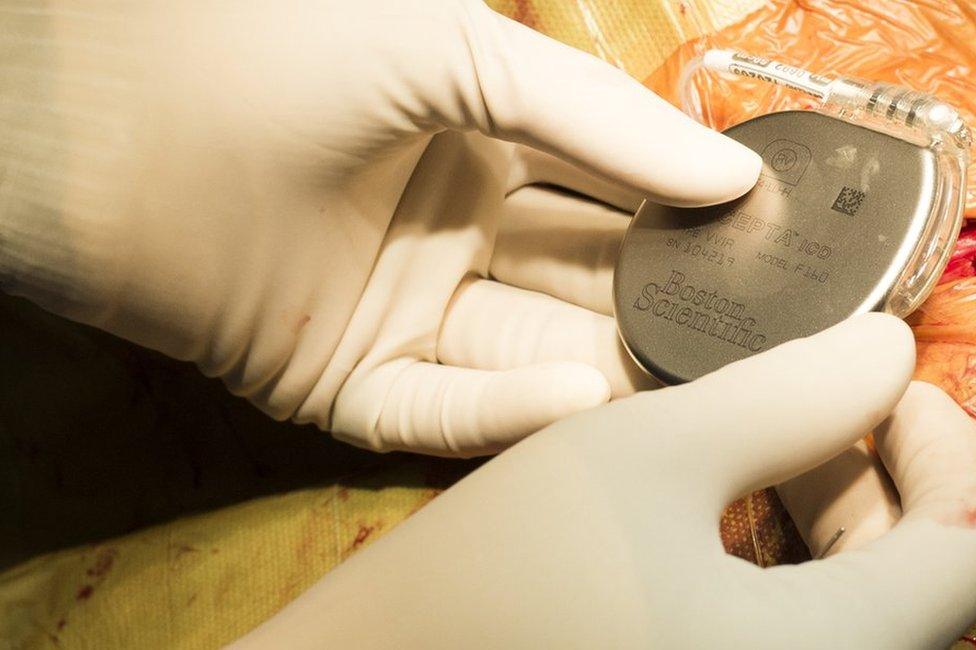
Pacemakers and ICDs

The first implanted pacemaker was given to Arne Larsson in Sweden in 1958, but the device failed after three hours
There is a difference between a pacemaker and other implanted heart devices, the most common of which are called implantable cardioverter defibrillators (ICDs)
A pacemaker sends regular electrical pulses to keep a heart beating steadily, while an ICD sends pulses only to correct an abnormal heartbeat
While some doctors have been asked to turn off ICDs at the end of life, Nina Adamowicz's case is the first known instance in the UK of a request involving a pacemaker

As for Nina Adamowicz, despite her hospital trust's initial hesitation, her request was finally granted in October of last year - after meetings, legal consultation and psychological testing to establish that she fully understood the consequences of her request.
More than 35,000 people in the UK had pacemakers fitted in the last year, and many in the medical profession are now urging doctors to talk to their patients with pacemakers about their wishes as they approach the end of their lives. Although he isn't giving interviews, Adamowicz's doctor says it's a case he'll never forget. He has been presenting the case at local medical talks and events, which he says generates considerable debate. Some of his colleagues support the decision while others feel it's uncomfortably close to euthanasia.
Adamowicz went into her local hospice with her family and lay chatting while her doctor turned the pacemaker off, a procedure that took 20 minutes. She soon said she felt different, family members say. She described her body as feeling heavy and she felt a little nauseous, but said she felt at peace. She slept through the night, returned home in the morning and died later that night.
"I strongly believe I have the right to decide whether I want it on or off," she told iPM in that earlier interview. "And I stand by it."
'I have the right to decide', Nina wishes to turn her pacemaker off and be allowed to die.
Join the conversation - find us on Facebook, external, Instagram, external, Snapchat, external and Twitter, external