PMDD: Pain, panic attacks and having my womb removed at 22
- Published

Nichole's PMDD symptoms were so severe she had to have a hysterectomy
Nichole started her period aged 12. For the next eight years, she felt her monthly suicidal thoughts, depression and rage were normal.
They weren't.
From her first period, Nichole, from Stoke-on-Trent remembers having breakdowns, panic attacks and flying into rages.
"I'm not ashamed to admit that because that's part of the illness for me," she tells BBC Newsbeat.
But Nichole had to wait until she was 20 to give the condition a name - premenstrual dysphoric disorder, or PMDD.
It's a very severe and intense form of premenstrual syndrome (PMS), but can have a much bigger impact on your quality of life and daily routine.
Symptoms vary and some experience them more severely, but they tend to be include extreme mood swings, irritability, tiredness and losing interest in usual activities.
And, like Nichole, many face a long wait for a diagnosis.
It's thought about 5.5% of women are affected and high-profile names like Vicky Pattison, Zara Larsson and Dixie D'Amelio have shared their experiences with the condition.
The cause is unknown, but the NHS says it could be genetic.
Nichole says it affected her like an allergy, with her brain reacting negatively to hormone changes in her menstrual cycle.
'I wanted my life back'
At her lowest, Nichole, who's now 25, says she tried to self-harm in "the worst episode" she's ever had, and had to go to hospital for her own safety.
"I said to my surgeon, 'I know that I'm going to try and do something stupid when I have another episode' and I didn't want to do that," she says.
"I didn't want to die."
Figures from IAPMD, an organisation which campaigns for better awareness of menstrual health, estimate almost 50% of women, external who have PMDD have planned a suicide attempt.
After trying multiple treatments that didn't work, like the contraceptive pill and hormonal therapies, Nichole consulted her gynaecologist and realised her only option was a hysterectomy.
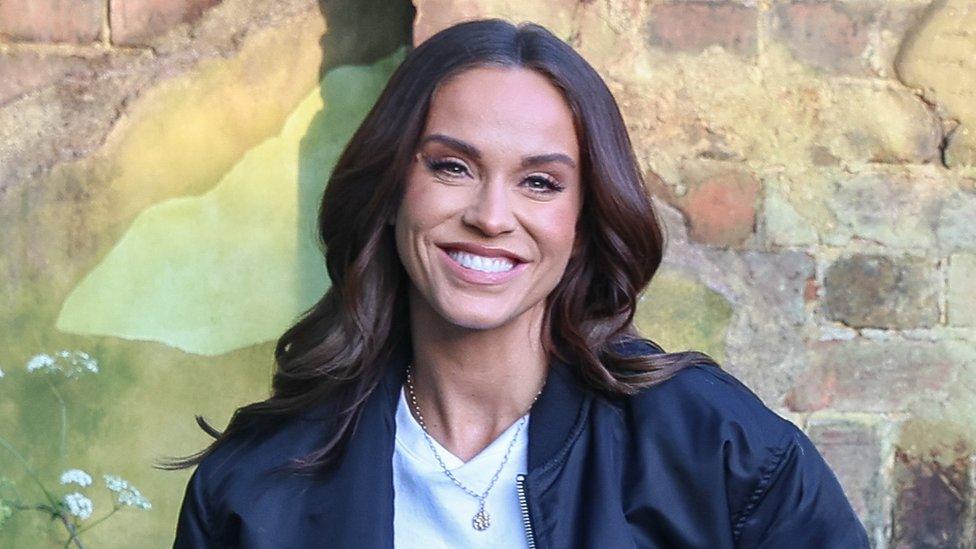
TV star Vicky Pattison has opened up about her PMDD diagnosis in conversation with Radio 1
In 2021, she had her womb, cervix and both ovaries removed.
"I struggled with the fact that I'll never have kids of my own," she says.
But the alternative was to continue the suffering, and Nichole says she couldn't consider that.
"As a 22-year-old who had been going through it since I was 12 - 10 years of pure hell - I needed my quality of life back."
'You know your body best'
Nichole says the link between mental and menstrual health needs to be better understood.
Before her symptoms were connected to her periods, doctors tried putting her on antidepressants, even though at times in her cycle she was "absolutely fine".
Dr Nighat Arif is a GP specialising in women's health and says PMDD symptoms often overlap with mental health issues.
"It's really common for young girls to get fobbed off and be told it's a mental health condition, when actually that's not the case," she says.
"The symptoms to look out for are emotional changes such as extreme mood swings, tearfulness, sudden extreme sadness, irritability or anger, depressed mood, or even suicidal thoughts.
"Once your bleed has happened, the person then feels they're back to their regular self."

Nia Crockford says she tried lots of treatments including the contraceptive pill before undergoing chemical menopause
Although there's no cure and symptoms vary for different people, 26-year-old Nia Crockford has been able to manage her PMDD through chemical menopause.
She first noticed symptoms when she was 18 but "was always told it's just a painful period".
"I can wake up one day and suddenly I don't feel like I'm the same person. Then it disappears as my period comes. I have a few weeks of being fine and it will start all over again."
The treatment she's on involves hormone injections to mimic menopause, which normally happens to women in their 50s, and causes your periods to stop.
It's reversible so Nia has the option to have children in the future and she feels it's a "complete game changer".
Although similar treatment didn't work for Nichole, Nia says it's helped her live "like a normal 20-something" and given her emotional stability.
It can take an average of 12 years to be diagnosed with PMDD and Dr Arif says anyone who thinks they might be affected should speak to their GP.
She suggests keeping a symptom diary and tracking your symptoms against your period, which can help identify it.
"You know your body best," she says. "Understanding that it's happening in around your periods is really important."
Newsbeat has approached the NHS for comment.
If you have been affected by the issues raised in this article, help and support is available via BBC Action Line.
You can also speak to your GP, call the NHS on 111 or contact Samaritans., external


Related topics
- Published2 August 2023

- Published18 October 2023

- Published28 July 2020

- Published28 July 2020
