Parasite may aid cattle TB spread
- Published
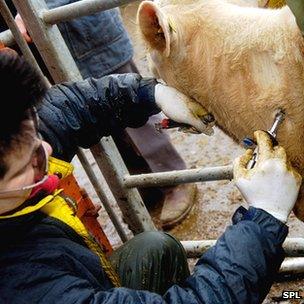
TB testing has been stepped up recently - but liver fluke may make it less effective
The spread of an animal parasite across the UK may be hampering moves to curb cattle tuberculosis, research suggests.
Scientists have known for a few years that cows carrying both TB and the fluke <italic>Fasciola hepatica</italic> are less likely to show positive on the normal TB test.
Now researchers have shown that this could lead to a reduction of one-third in the detection of infected cattle.
Cases of bovine TB soared over the last decade, leading to tighter restrictions on farmers and a possible badger cull.
The disease now costs the UK public purse more than £100m per year.
Some of that is spent on regular testing of cattle herds for TB; but the new research, reported in <link> <caption>Nature Communications journal</caption> <url href="http://www.nature.com/ncomms/index.html" platform="highweb"/> </link> , suggests the testing is being compromised by presence of the liver fluke.
It has been known since at least 2006 that under experimental conditions, infection with <italic>F. hepatica</italic> lowers a cow's reaction to the skin test.
The 3cm long parasite fends off the cow's natural defence mechanisms by "turning down" its immune system.
The TB skin test relies on detecting an immune response to a harmless part of the TB bacterium. With the cow's immune system suppressed, the response is not as strong.
More is less
The new research takes this lab result into the real world of farming by looking at the relationship across the UK between levels of liver fluke infestation and rates of TB diagnosis.
"We started this work thinking that infection with the liver fluke might make animals more susceptible to pathogens that are normally controlled by an inflammatory immune response, and TB is the obvious one to think about," said research leader Diana Williams from the University of Liverpool.
"We were surprised, because we suspected there would be a TB increase in cattle infected with fluke; but what we found from the data was a negative association - more fluke, less apparent TB."
Using a computer model relating disease incidence to environmental conditions such as temperature and rainfall, the researchers concluded that TB ought to be present in areas where it was not showing up.
Their conclusion is that the sensitivity of the test in picking up TB infection is reduced in areas where lots of cows carry liver fluke.
Prof Williams also said fluke had become more common in the UK over the last 15 years - the very period that has seen a tripling in the number of cattle herds where TB is present.
Flukes may be thriving partly because of climate change, she suggested, but also because of agri-environment schemes that encourage farmers to maintain ponds, lakes and marshes to support wildlife.
<italic>F. hepatica</italic> spends part of its life cycle in snails, which thrive in warm, wet conditions.
Policy time?
If the chances of detecting TB through the skin test really do go down by a third, as the researchers conclude, that would mean infected cattle are not being detected during routine testing - which in turn means they can infect other cows in the same herd and be eligible for transport from farm to farm.
Carl Padgett, president of the British Veterinary Association, described the findings as "important research".
"The skin test for TB has been proven to work well at eradicating infection in cattle throughout the world," he said.
"It is important to recognise its imperfections to maximise its value in the continued efforts to eradicate this disease."
Epidemiologist Prof Christl Donnelly from Imperial College London, a former member of a government advisory panel on bovine TB, said that if confirmed, the findings could lead to useful policy changes.
"It's potentially really interesting - anything that can explain where test sensitivity is going wrong is potentially very useful in finding out where the cattle test might be doing less well," she told BBC News.
"I think it would definitely be worth following up and asking whether there's any effect of liver fluke on gamma-interferon (another type of TB test) - and if the answer is 'no', maybe there should be more use of gamma interferon in those areas."
But the Department for Environment, Food and Rural Affairs (Defra) played down the significance of the finding.
A spokesman pointed to another line of research pursued by the Liverpool-led team, in which cattle had been infected in experimental conditions with both liver fluke and the TB-causing agent <italic>Mycobacterium bovis</italic>.
All cows showed a depressed response to the skin test - but not so much that the test would not have picked them up.
"This research shows that cattle who have both liver fluke and bovine TB still test positive for bovine TB, and would be culled to control the disease," he said.
"The absence of positive cases of bovine TB in some areas co-inciding with large amounts of liver fluke cannot be used to claim liver fluke is hiding cases, as cattle carcasses are inspected in abattoirs and we would see evidence of TB in the slaughtered animals if this was the case."
However in farm conditions, where cows may carry a heavier load of fluke, it is possible that the skin test would fail to produce a response, the researchers say.
Everybody agrees that the case is not proven by this one piece of research, and Prof Williams said more needed to be done to understand the real situation on farms and also look for ways to respond.
"Fluke infestation is quite seasonal - we tend to see it occurring towards the end of the summer, and so by controlling access to marshy pastures or fencing off marshy areas, farmers could reduce the risk of infection," she said.
The picture is somewhat clouded by the fact that resistance is emerging to triclabendazole, a commonly used drug against fluke.
In addition, the European Medicines Agency recently restricted use of ivermectin, a drug often used in combination with anti-fluke agents in broad parasite formulations, after the UK raised concerns that its presence in cow's milk could pose a threat to human health.
The research will inevitably raise anew the question of whether badger culling, which Defra wants to see started later this year, is really needed.
Follow Richard <link> <caption>on Twitter</caption> <url href="http://twitter.com/#!/BBCRBlack" platform="highweb"/> </link>
- Published17 May 2012
- Published20 April 2012
- Published20 March 2012
- Published12 October 2011