Microneedle sensor aims to cut hospital superbugs
- Published

Regular blood tests are typically used to monitor reactions to antibiotics and other drugs
Seriously ill patients could get help to recover more quickly thanks to a sensor that uses tiny needles to monitor medication.
A team at Imperial College, London, has developed the sensor, external that constantly samples patients' antibiotic levels.
The sensor can show how a patient has reacted to the type of antibiotic they have been given.
Experts said the technique showed promise but needed more work to make it reliable enough to use in hospitals.
But in theory, it has the potential to reduce the number of hospital superbugs.
Steady sample
Dr Timothy Rawson, who helped develop the sensor, said it had the potential to produce results much more quickly than current practice.
Existing methods of monitoring response to treatment tend to be slower and involve frequent blood tests, he said.
"By using a simple patch on the skin of the arm, or potentially at the site of infection, it could tell us how much of a drug is being used by the body and provide us with vital medical information, in real time," he told the PA news wire.
The sensor is the size of a small plaster that has tiny needles on its underside which can be coated with enzymes tuned to react to different drugs.
The needles are many times thinner than a human hair and are small enough to slip between skin cells. This lets them sample body fluids as they flow between cells.
The array of needles sample fluids 200 times a second and can detect tiny changes that indicate how patients are reacting after being injected with antibiotics.
The information the patch gathers could help ensure patients get the right amount of antibiotics and could swiftly spot adverse reactions, said the researchers.
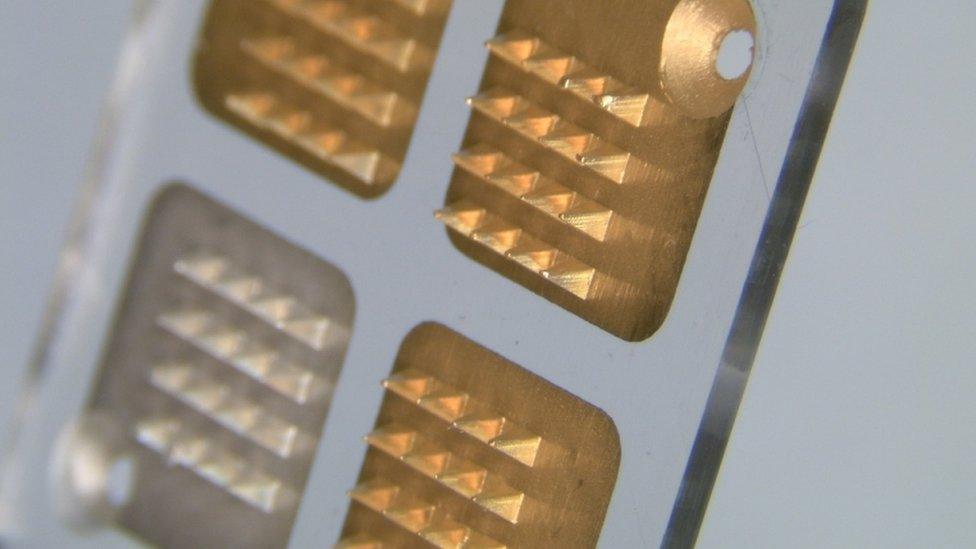
The tiny needles sample the flow of body fluids
The tests measured responses to penicillin but, said the researchers, the needles could be coated with enzymes for many different types of antibiotic.
Until now, micro-needle sensors have been used to monitor blood sugar levels but the Imperial work is believed to be the first use of such devices for monitoring antibiotic use.
Details of a small scale medical trial of the non-invasive technique have been published in the Lancet's digital health journal. The researchers said the sensor produced results close to the "gold standard" obtained by regular blood tests.
If future larger-scale tests proved successful, said Dr Rawson, the technology could help reduce drug-resistant infections, help manage serious infections and save the NHS money.
Aiden Doherty, group leader in biomedical data science at the University of Oxford, said the trial showed the "potential" of wearable sensors to continually monitor health without subjecting patients to unpleasant procedures.
However, he said, the research was an "early study" and a lot more work was needed to make the technology reliable enough for clinical use.
"Much larger clinical tests will be needed in specific patient populations too, such as those at risk of sepsis," he told the BBC. "So while encouraging, years of careful work are required before micro-needles can be routinely used in hospitals for antibiotic drug monitoring."
- Published26 September 2019

- Published13 September 2019

- Published22 August 2019
