Sex, drugs and A&E: 10 charts on how the under-30s use the NHS
- Published

Most of us make greatest use of the NHS at the beginning and end of our lives.
But although the 18-30s have youth on their side, their relationship with the NHS is still significant.
Since health is devolved, information on the NHS is collected separately by each UK country - but many of the trends found in England are similar to those of Scotland, Wales and Northern Ireland.
So how do young people shape the services supplied by the NHS and how has it shaped them?
1. Young adults are big users of A&E...
In 2016-17, 18- to 29-year-olds made 3.9 million visits to accident and emergency units in England, representing 20% of all visits - this is despite representing just 16% of the population as a whole.
Young adults are one of only two adult groups in England whose use of A&E is proportionately higher than their population, the other being over-65s.
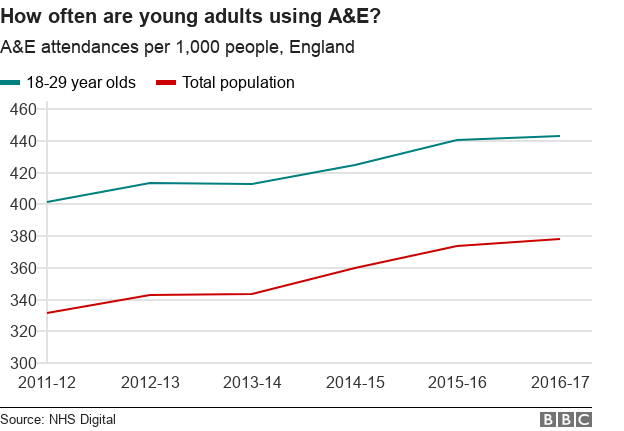
Among young adults, this need for urgent care might reflect more active, sometimes chaotic, lifestyles, with high admissions due to sporting accidents, violence and alcohol-related incidents.
2. ...but are using other hospital services less
While young adults might be more likely to visit A&E, their overall engagement with hospitals is considerably less.
With less need for major procedures and repeat visits, 15- to 29-years-olds account for just 10% of hospital "episodes" in England.
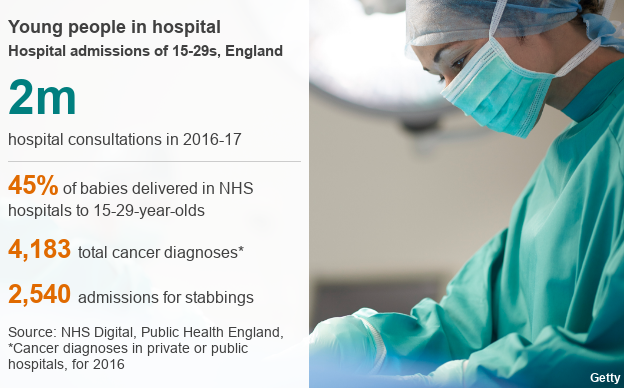
And most of these visits are by women, partly explained by the role hospitals play in pregnancy and maternity issues.
Also, 15- to 29-year-olds have less need for longer-term treatments. In 2016, for example, this group accounted for under 2% of new cancer diagnoses in England.
3. They are less likely to see their GP
GP attendance statistics have not been collected by NHS England since 2008, but we do have 2013 statistics from NHS Scotland, which show that GP visits increase with age.
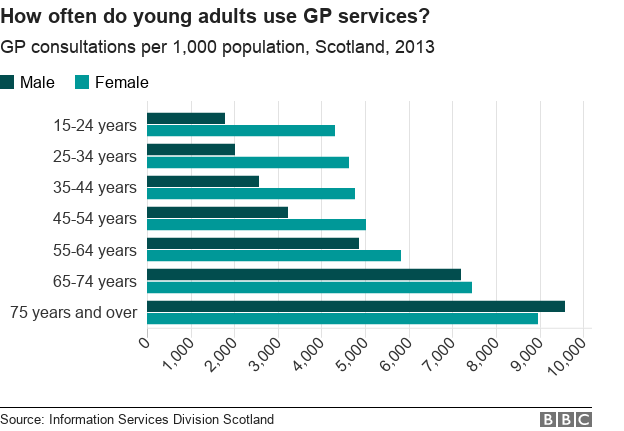
Young women are more than twice as likely to visit than men.
Cervical cancer screenings and contraceptive services will play a part in this gender gap.
4. Their lifestyles are getting better
In some key areas, young adults are moving away from unhealthy habits such as drinking and smoking.
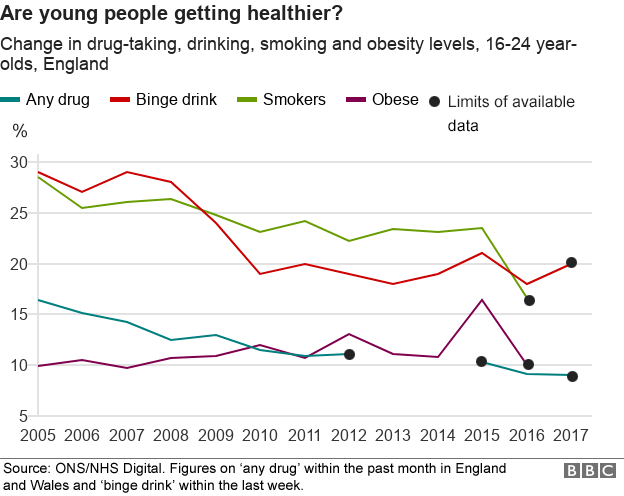
Public health campaigns, such as NHS England's Smokefree, external - and equivalent programmes in Scotland, Wales and Northern Ireland - have long aimed to reduce the prevalence of these habits.
This doesn't just improve health but also reduces the economic burden placed on the NHS.
5. And drug addiction treatments are dropping
Last year, there were 40,385 people between the ages of 18 and 29 receiving treatment for drug problems across England.
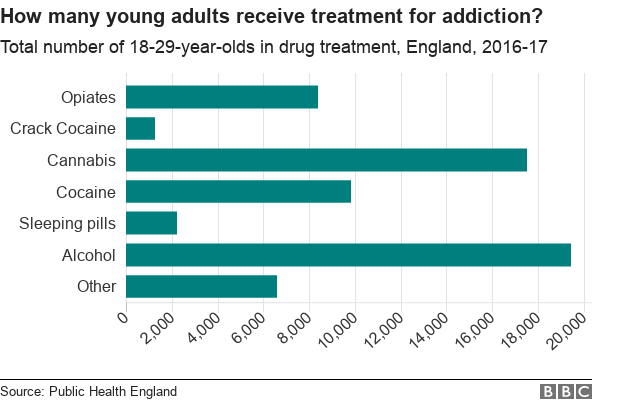
Public Health England suggests this is in part due to declining use of drugs by the age group, but over the period drug services have also been cut.
Overall drug treatment is highest among people in their 30s, but 18- to 29-year-olds were the most likely to receive help for cannabis use - there were 11,200 new patients last year.
Interventions can include inpatient detoxification, self-help and medicinal treatment.
6. They have benefited from health changes
A hundred years ago, the top 10 causes of death in England and Wales included pneumonia, epilepsy, diphtheria and scarlet fever.
But improved healthcare and scientific innovation over the intervening decades have helped ensure that young people are less likely to have - or eventually die from - life-altering diseases or infections.
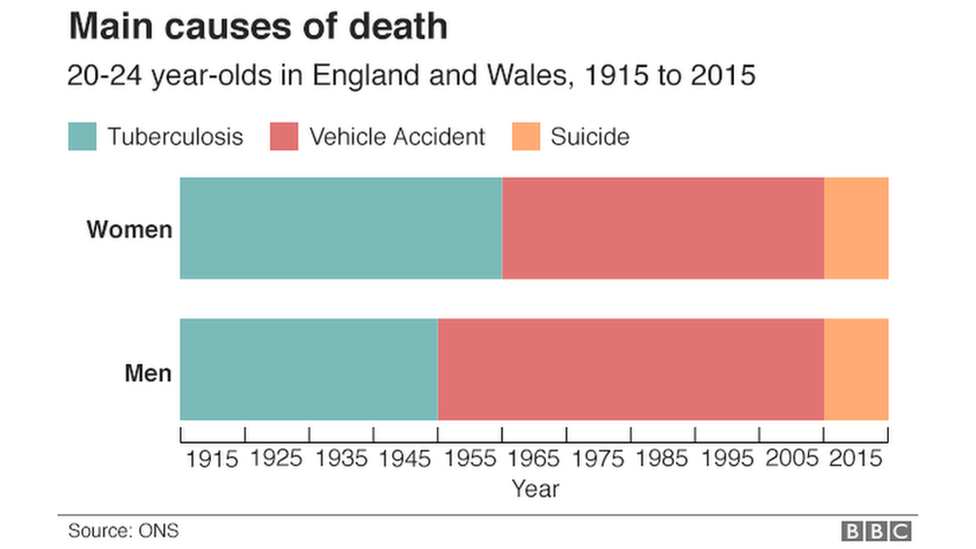
Today, the biggest killers tend to be injury or self-harm.
This has highlighted modern public health issues including violent crime - the fourth biggest killer of young men - and mental health.
7. Young women receive most mental health support
According to the NHS's mental health survey, young women in England are the most likely group to have mental health problems.
Roughly a quarter of women aged 16 to 34 have a common mental health disorder, a problem that has increased over time.
Not everyone seeks help for these problems, but when necessary doctors can refer them for "talking therapy".
Not all referrals will receive "talking therapy", with some requiring more intensive treatment.
And other referrals will not result in treatment because patients may opt out.
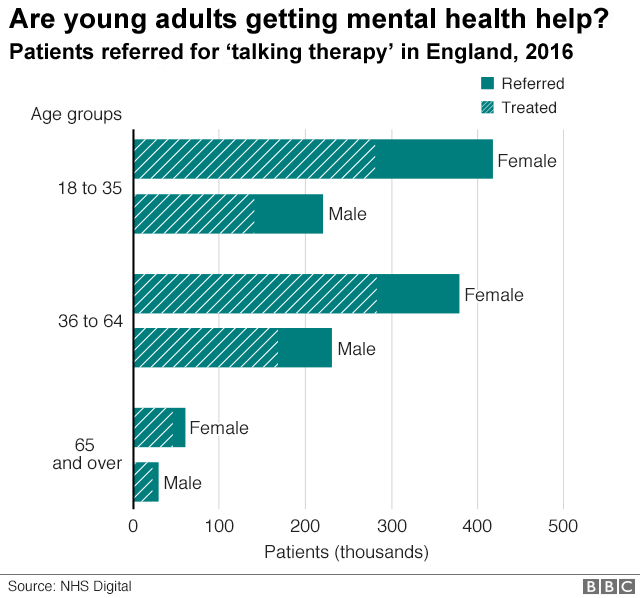
Efforts have been made to increase awareness and accessibility to mental health services in recent years.
For example targets have been introduced aiming at ensuring those with their first case of psychosis are seen within two weeks, but these aren't always being met.
8. Young adults dominate sexual health service usage
Last year in England, 814,479 young adults aged between 18 and 34 used face-to-face sexual health services.
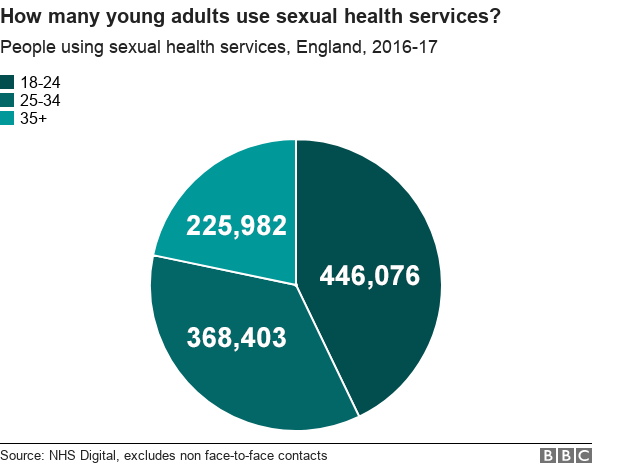
Over a third of users were aged between 18 to 24, of which 90% were women, usually consulting about contraception.
In recent years, face-to-face consultations have decreased as more information and services are made available online.
Over this period, sexually transmitted infections have decreased - but recent increases in syphilis and gonorrhoea have raised concerns about changes in sexual practices.
9. They cost the NHS relatively little to care for
The Department of Health spends £124bn a year on health in England, most of which goes directly to NHS England.
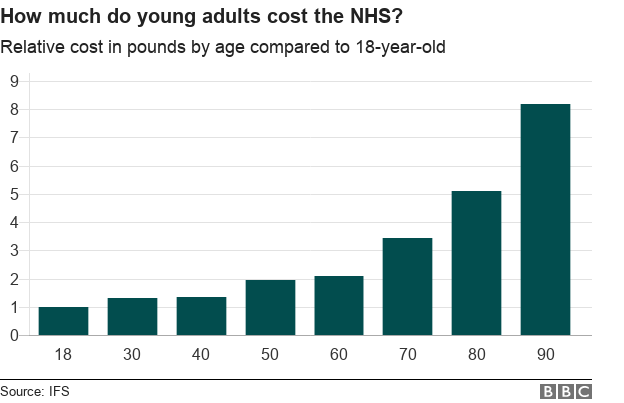
Given that young adults tend to have more short-term health problems, they are relatively inexpensive to treat. The general trend is the older you get, the more expensive treatment is.
The average working 24-year-old in England will pay about £340 in tax towards health each year.
10. They are supportive of the way the NHS is run
Young adults in England tend to be supportive of the way the NHS is run, but no more so than the rest of the population.
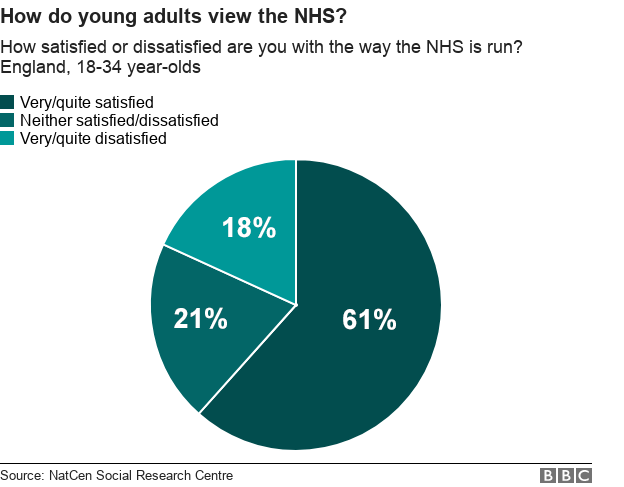
According to the NatCen Social Research, 61% are very or quite supportive of the running of the NHS, compared with 63% of the total population.
When asked if they were willing to pay more in taxes to support the NHS, 19% of young people said they would, and 31% said they would support a new NHS ring-fenced tax.