'It's like Michael walking into a fog'
- Published
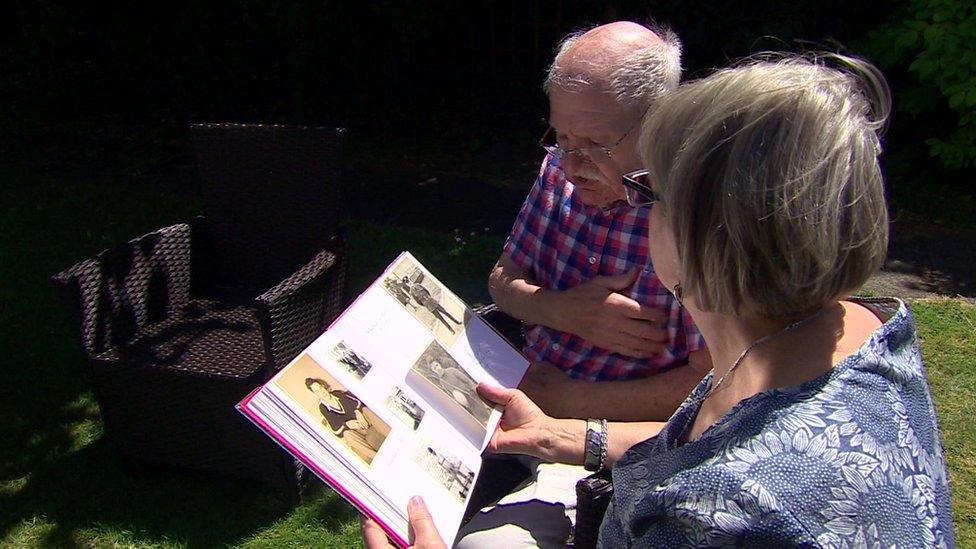
Lynda Basford cared for her husband Michael at home for 13 years until last year
"It is like Michael walking into a fog," says Lynda Basford, describing the 13 years during which her husband Michael has descended into dementia.
She has been at his side throughout.
"You can't quite hold on to him," she says, "and as the years go by, he gets deeper and deeper into that fog and you can't do anything about it."
Michael needs a lot of support. He doesn't really know where he is and he no longer recognises his wife. Even remembering to eat requires encouragement.
She looked after him for years in their own home with little support but, last year, it all became too much.
She felt she could no longer keep him safe and reluctantly agreed he should move into a residential home.
However, the financial support they get from their local authority does not cover the cost and their savings are rapidly disappearing.
Now Lynda's strain over her husband's condition is compounded by money worries.
"I didn't realise", she says, "that if you have a terminal illness, your level and quality of care would be dependent on your bank balance."
Lynda Basford: "Because he drew the short straw... he's having to pay for his treatment."
A new report produced for the BBC from the Health Foundation and three other leading research organisations says the failure by successive governments to reform social care has left many people without the support they need in care homes or in their own homes.
It describes the current council-run means-tested system as a fundamental source of unfairness.
An ageing population, more younger people with disabilities needing support, and budget cuts combine to leave local authorities struggling to meet the demand for help.
The report highlights how budget pressure means the social care system is nearing crisis:
councils already have to focus spending on people with the most severe needs
400,000 fewer people received publicly funded care in 2014 than in 2010
the funding shortfall is expected to reach £18bn by 2030
almost 7% of care worker jobs were vacant last year
The report says this means that three-quarters of relatives of people who need care at home get no support and have not been able to take a respite break of even an hour from caring in the last 12 months.
Lynda Basford questions why the support Michael needs is not provided by the NHS.
"Michael has drawn the short straw and has dementia and not some other terminal illness, so he is having to pay for his treatment - because his treatment is social care," she says.
Michael gets some help from his local authority because he has less than £23,250 in savings, but the rate the council pays does not cover the £800-a-week fees of the care home.
It means that each week, Lynda pays £550 from their savings to make up the difference. She says it is only a matter of time before they run out of money and then she does not know what will happen.
Means-tested care
Next week, like the NHS, the care system will mark its seventieth anniversary.
While the health service was set up as a separate institution delivering support that is free to those who need it, from the start services provided by councils for people struggling with daily tasks such as washing, dressing and taking medication, were means-tested.
But in 1948, people did not survive with the sort of complex conditions that meant long-term social care was needed in the way it is now.
Then, charities like the Alzheimer's Society did not exist - it was established 40 years ago because of the increasing number of people with dementia.
The society's chief executive Jeremy Hughes says: "When the funding system was set up in 1948, no-one intended to set up a separate system for one disease rather than another, we've got that by accident rather than design. It needs to change now if we are going to be fair and equitable for people over the next 10, 20, even the next 70 years."

The couple have been together for 40 years
Last week, after announcing more money for the health service, the government said it was delaying the publication of long-awaited plans for the funding of the social care system until the autumn.
Jennifer Dixon, chief executive of the Health Foundation, welcomed the extra cash for the NHS, but pointed to the urgent need for more money for social care.
"The NHS was founded 70 years ago to replace fear with security, so that people did not face bills they couldn't pay in time of illness.
"But that security is just not there for many of those who need social care today," said Ms Dixon.
"Many people assume social care is free of charge like the NHS, and it is a huge shock when they find out it isn't and the bills mount up.
"As local authority budgets are squeezed, more people are having to go without, pay themselves or rely on unpaid care from friends and families. The situation is unfair, stressful and inefficient and is long overdue for reform."
In a statement, the Department of Health and Social Care said it recognised the social care system was under pressure and reforms would "ensure it is sustainable for the future".
"Health and social care are two sides of the same coin and any reforms must be aligned. That's why our forthcoming Green Paper will be published in the autumn, with the NHS plan.
"We have provided local authorities with £9.4bn in dedicated funding for social care over three years and will agree a sustainable funding settlement at the forthcoming spending review."