'Last embryo' baby boy born after 15 rounds of IVF
- Published

Matheson Calon Tallett Vaughan Jones was born on 10 December
A couple has brought home a healthy baby boy who was the "very last embryo" they implanted after deciding to call time on their attempts at IVF.
Lewis and Hannah Vaughan Jones spent £80,000 on 15 rounds of IVF after being told they would not conceive naturally.
They had decided that if the latest round of IVF did not work, they would give up on the treatment - but then Mrs Vaughan Jones became pregnant.
The couple, who are both TV presenters, said baby Sonny was "beautiful".
After about six years of an "all-consuming" emotional and financial struggle - and following medical advice - the couple decided to make a final attempt at IVF.
"We had zero hope... emotionally, we had already moved on," Mr Vaughan Jones said.
"We'd tried so many times and statistically it was so unlikely to work. And that's why we absolutely couldn't believe it when the very last embryo was the one that worked."
When Mrs Vaughan Jones, 38, became pregnant, her husband said he was "terrified" of another miscarriage.
He could not bring himself to buy baby clothes or redecorate their home in Twickenham, south-west London until more than six months into the pregnancy.
But Matheson "Sonny" Calon Tallett Vaughan Jones was born by Caesarean section on 10 December.
"It's been just as wonderful and crazy as you'd expect," Mr Vaughan Jones, who is also 38, said.

Hannah and Lewis attempted more rounds of IVF than many UK couples can afford.
The NHS limits how many cycles it offers to those who are eligible because of the price.
Costs vary, but one cycle of treatment may cost up to £5,000 or more.
Guidelines for the NHS recommend three cycles, but some NHS trusts offer less than this.
There is no set cut off if you go private and have enough viable eggs and time to keep trying, although doctors would and should advise you to stop at some point - when they think the odds of success are too low to merit continuing.
In general, the chances of IVF working decrease with age if the couple are using their own eggs and sperm rather than donor ones.
If you are having trouble getting pregnant, you should speak to your GP, who can refer you to a fertility specialist.

Mr Vaughan Jones, a presenter for the BBC News channel, said he and his wife "knew how lucky we were that we've both got good jobs" and could afford repeated rounds of IVF after one unsuccessful attempt paid for by the NHS.
But he added that the couple had felt "cheated" and "emotionally vulnerable" every time they handed over more money.
Mrs Vaughan Jones, a news anchor for CNN, first spoke openly about the "hell" of IVF in an article for the Times in 2017, external.
She described the article as being a "sort of 'coming out'" because "there was so much shame or stigma attached to infertility".
Mrs Vaughan Jones said friends told her writing the article was "a brave thing to do", but that to her it felt "purely self-indulgent" as it was like "free therapy".
Allow X content?
This article contains content provided by X. We ask for your permission before anything is loaded, as they may be using cookies and other technologies. You may want to read X’s cookie policy, external and privacy policy, external before accepting. To view this content choose ‘accept and continue’.

After Mrs Vaughan Jones's article, the couple documented their IVF journey in various ways, including uploading video diaries to YouTube to show others what the treatment involved.
Mr Vaughan Jones said that while he was normally quite a private person and had felt "nervous" about his wife's article, he also recognised the importance of speaking out.
"We didn't see anyone talking about just how low, bad and difficult [IVF] is," he said.
Mrs Vaughan Jones said she hoped by opening up about her family's journey, she could persuade others to do the same.
"I encourage people, even if they're naturally quite shy, to talk to someone, even if it's a stranger or the wonderful online community… to just understand that you're not alone and there is support out there."

In Vitro Fertilisation (IVF)
In IVF treatment, an egg is removed from the woman's ovaries and fertilised with sperm in a laboratory.
The fertilised egg is then returned to the woman's womb to develop.
IVF worked for the first time on 10 November 1977. On 25 July 1978, the world's first IVF baby, Louise Brown, was born.
On average, IVF fails 70% of the time. The highest success rates are for women under 35, where a third of treatment cycles are successful.
On average, it takes almost four-and-a-half years to conceive with IVF.
Source: Human Fertilisation and Embryology Authority/Fertility Network UK

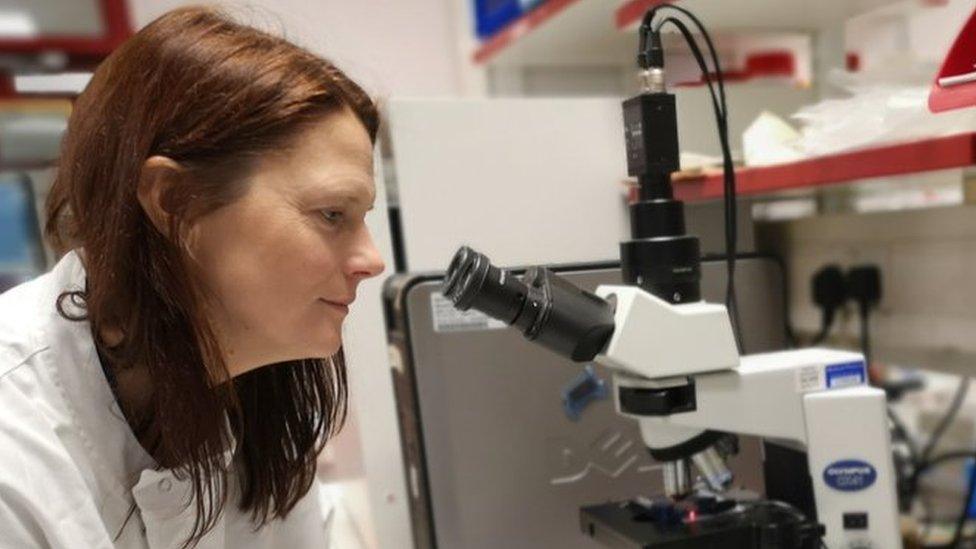
Fertilisation expert Dr Carol Lynn Curchoe said there had always been "a general idea" in her field of research that increasing rounds of IVF give infertile couples a greater chance of success - and that her own recent research, external found this was the case for some types of treatment.
Dr Curchoe added: "Having success after 15 rounds of IVF is an extraordinary accomplishment and shines a bright light on the miracles that can and do happen when doctors and patients don't give up."
- Published5 December 2019

- Published30 October 2019

- Published29 October 2019
- Published27 October 2019
