Endometriosis care needs urgent improvement, MPs say
- Published
Living with the 'invisible pain' of endometriosis
Endometriosis care across the UK needs urgent improvement and diagnosis times need to be cut in half, a report by MPs says.
It found an average wait for a diagnosis was eight years and that has not improved in more than a decade.
Endometriosis affects one in 10 women in the UK and can cause debilitating pain, heavy periods and infertility.
Nadine Dorries, minister for women's health said awareness was increasing but there was still a long way to go.
More than 10,000 people took part in the All-Party Political Group inquiry which found that 58% of people visited the GP more than 10 times before diagnosis and 53% went to A&E with symptoms before diagnosis.
The majority of people also told MPs their mental health, education and careers had been damaged by the condition.
About 90% said they would have liked access to psychological support but were never offered it, with 35% having a reduced income due to endometriosis.
There is no cure for the condition and treatment can include hormone therapy and surgery.

Sarah Smallbone had four operations in three years to alleviate symptoms
Sarah Smallbone, 37, from Essex, who gave evidence to the inquiry, was diagnosed with endometriosis aged 30 and had four operations in three years. She worked at a supermarket, but quit as her condition got worse.
"Endometriosis is life-changing. The pain can be so varied but at its worst, it is crippling to the point that the strongest painkillers only seem to make me drowsy," she said.
"After several warnings for my sickness, the final straw was returning from surgery, which ended up causing me kidney failure, and being given an official disciplinary. Knowing that I still needed another operation to reverse my bowel, I felt I had no choice but to quit."

'We can't carry on like this'
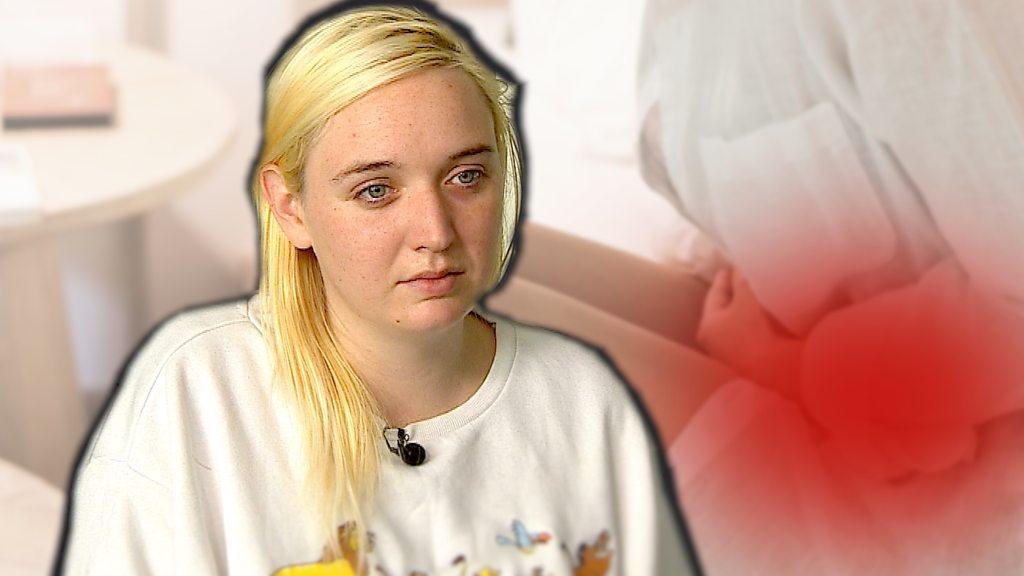
Helen-Marie Brewster said the condition led to her getting poor GCSEs
Helen-Marie Brewster, 28, from Hull, has been told by doctors that her only remaining treatment option is a full hysterectomy.
She had symptoms throughout secondary school but was only diagnosed when she left education.
"I failed most of my GCSEs because I was in bed, in crippling pain. I've lost nearly every job I've ever had because of my poor attendance," she said.
"GPs ask me to explain to them what endometriosis is, because they don't know. They're the ones who are meant to help.
"Last year I visited the A&E department 17 times trying to find help and pain relief for this condition, even for just a few days so I can keep going.
"The wait time for diagnosis is so long that in that time it's spreading and doing more damage the longer it is left untreated... We can't carry on like this."

'I was fighting to be heard'

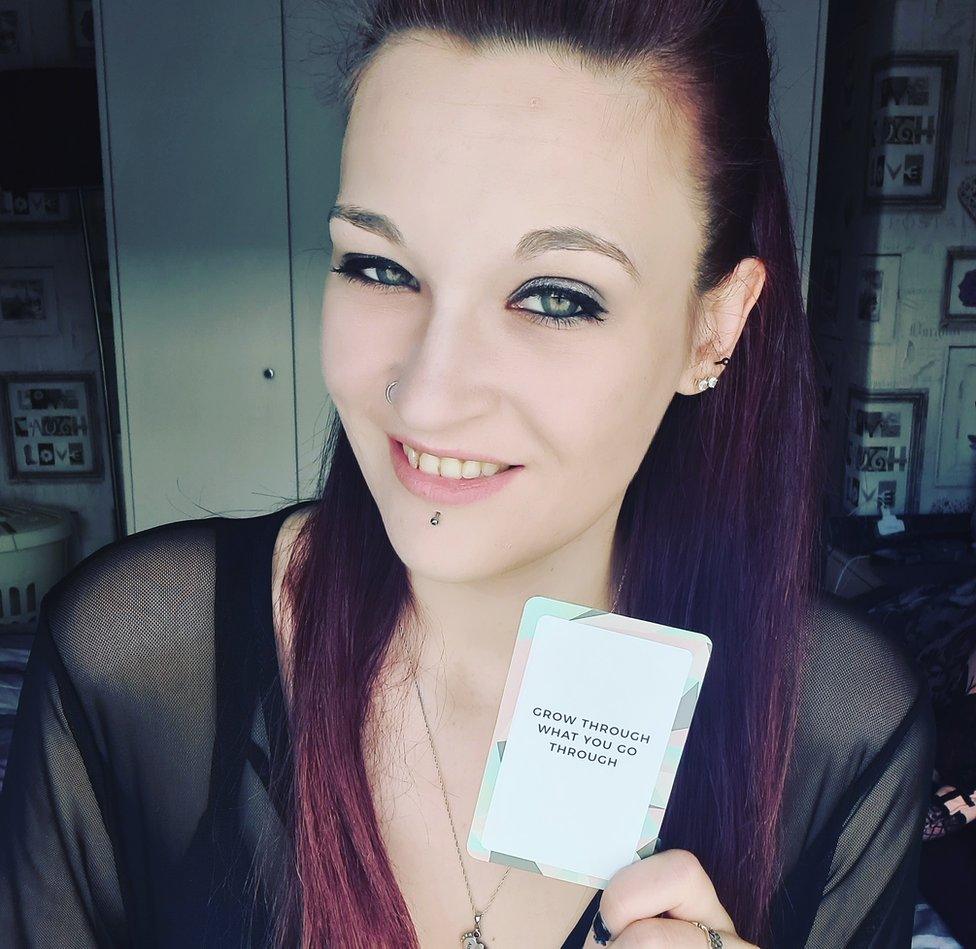
Natalie Meagan-Blake had to change her doctor four times before she was listened to
Natalie Meagan-Blake, 37, who was diagnosed four years ago, said there were further barriers for those from black, Asian and minority ethnic communities.
She says she had to change her doctor four times before she was listened to and referred to a gynaecologist. Then for her surgery she was missed off the operation list twice.
"The majority of black women and transgender men I've spoken to have had poor treatment, but you speak to other women and they're like, 'Yes, I have an appointment'."
The report calls for the government to investigate these health disparities and end the ethnicity and gender gaps in medical research.
It also recommends all UK nations have compulsory menstrual wellbeing on the school curriculum so young people know the warning signs and know when to seek help.
It is compulsory in schools in England from 2020, but is not currently UK-wide.
The report also calls for training to be reviewed for GPs, nurses and gynaecologists and for investment in research to find a cure.

What is endometriosis?
It is where tissue similar to the lining of the womb grows elsewhere in the body - often around the reproductive organs, bowel and bladder
Like the womb lining, the tissue builds up and bleeds every month but, with no way to escape the body, the blood is trapped, leading to inflammation, pain and formation of scar tissue
For some women there are no symptoms, but for others it is debilitating and can cause chronic pelvic pain, painful sex, painful bowel and bladder movements, fatigue and difficulties getting pregnant, external

Conservative MP Sir David Amess, who chaired the inquiry, said: "It is not acceptable that endometriosis and its potentially debilitating and damaging symptoms are often ignored or not taken seriously - or downplayed as linked to the menstrual cycle and periods."
Edward Morris, president of the Royal College of Obstetricians and Gynaecologists (RCOG) said: "The long diagnosis times and poor patient experience could be attributed to the significant gap in data when it comes to women and girls.
"The RCOG would like to see medical research in this area prioritised."
Nadine Dorries, minister for women's health, said it should not be the case that women have to wait so long to be diagnosed.
"While awareness of this, and other painful and potentially debilitating gynaecological conditions are increasing, there is still a long way to go," she said.
"I am committed to filling the evidence gaps to better understand the issues facing women and improve women's health. We have provided £2m, through the National Institute for Health Research, to investigate the effectiveness of surgery compared with non-surgical interventions to manage chronic pain in a specific type of endometriosis.
"Clinicians have a vital role in removing the stigma associated with endometriosis and I would urge them to follow the NICE guidelines, and to do all they can to support the mental and physical health of those suffering from this condition."
- Published18 August 2020

- Published3 March 2020

- Published7 October 2019
- Published6 October 2019

- Published6 October 2019
